Altering a patient's gut microbiome through fecal transplant improved response to immune checkpoint inhibitor therapy in 40% of patients with advanced melanoma who initially did not respond to the immunotherapy in a small, single-arm clinical trial. Researchers reported the findings in Science.
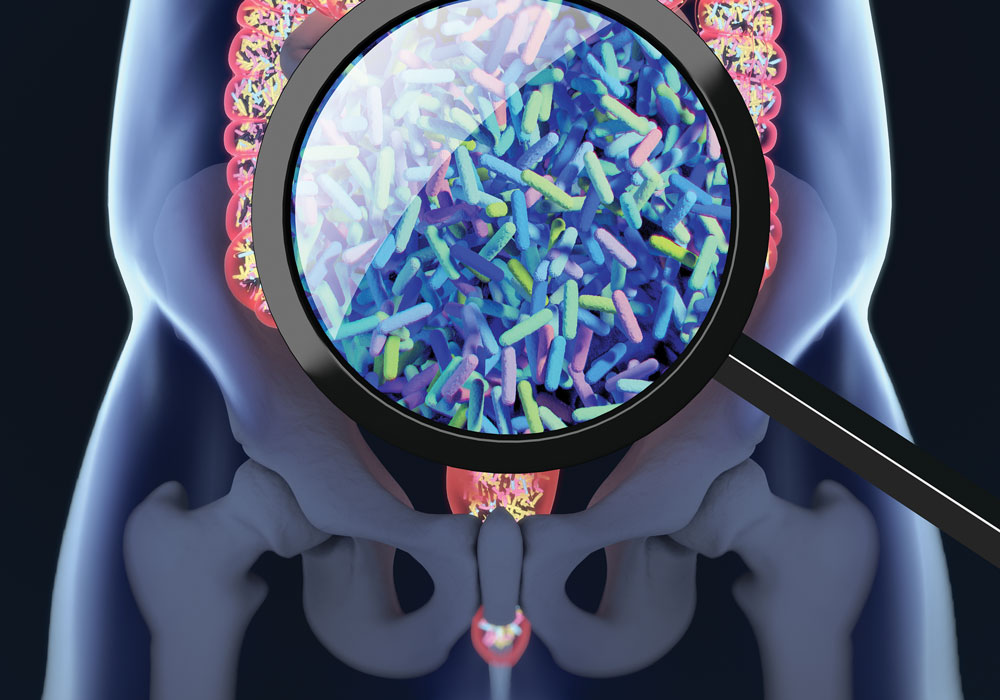
Only about 13% of patients treated with checkpoint inhibitors respond to the therapy, but researchers are searching for ways to overcome treatment resistance. In the new study, researchers took fecal microbiota from patients with advanced melanoma who had responded to pembrolizumab and transplanted it to the colons of 15 patients who had not originally responded to pembrolizumab or nivolumab. The nonresponders were then treated with pembrolizumab.
After the transplant and treatment, six of the nonresponders experienced either tumor reduction or long-term disease stabilization. In continued follow-up, one has had an ongoing partial response for more than two years and four others have had no disease progression for more than a year. An analysis of their gut microbiota showed bacteria associated with T-cell activation and immune checkpoint inhibitor response. Protein and metabolite biomarkers also demonstrated a systemic immune system response.
Larger studies are needed to confirm the results, and the researchers advised that those studies may lead to easier delivery methods for the specific microbiota each patient with resistance requires.
“We expect that future studies will identify which groups of bacteria in the gut are capable of converting patients who do not respond to immunotherapy drugs into patients who do respond,” the researchers said. “If researchers can identify which microorganisms are critical for the response to immunotherapy, then it may be possible to deliver these organisms directly to patients who need them, without requiring a fecal transplant.”