Since the first bispecific antibody (BsAb), blinatumomab, received U.S. Food and Drug Administration approval in 2014, the drug class has developed exponentially, with the majority of currently approved agents entering clinical practice in the past two years. BsAbs are very effective for treating certain malignancies, including multiple myeloma and leukemia, and most are approved for oncology indications. Here’s what makes BsAbs different than other cancer treatments and the key considerations for oncology nursing clinical practice.
Mechanism of Action
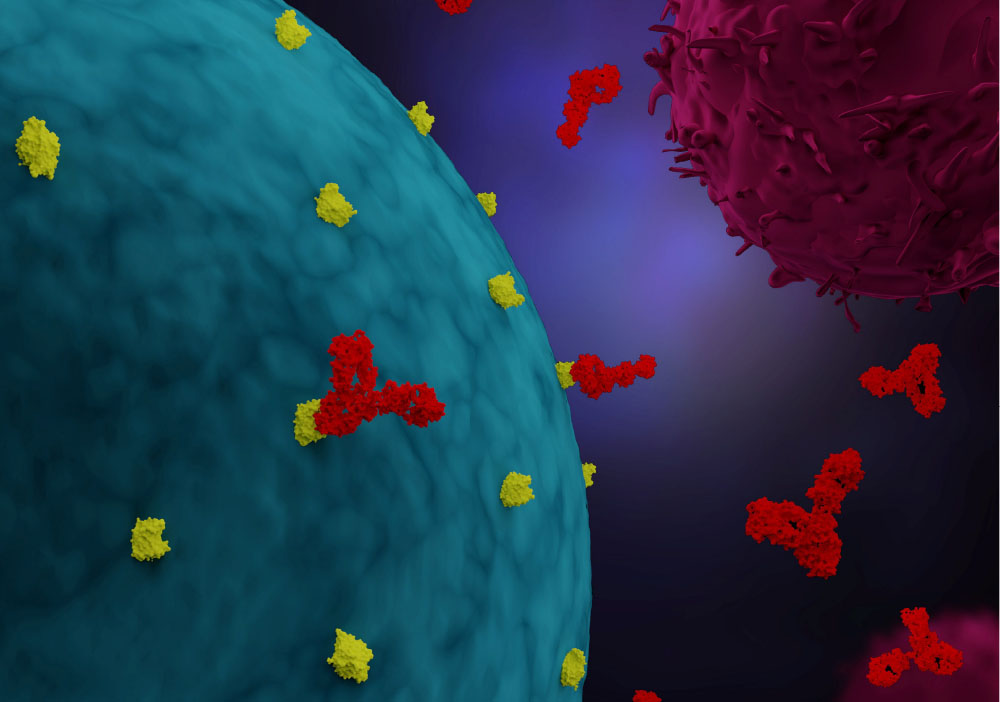
BsAbs are composed of two different monoclonal antibodies (mAbs). An mAb can attach to only one type of target at a time, but BsAbs attach to two different targets simultaneously. BsAbs generally serve as bridges for one of three pathways:
- Cells: BsAbs can bind to a specific antigen on tumor cells and to a different antigen on immune cells (e.g., cytotoxic T lymphocytes, macrophages). An example are the bispecific T-cell engagers, which bind to CD3 on T cells and a target on tumor cells (e.g., CD20 on malignant B cells), resulting in T-cell activation, cytokine release, and tumor cell death. This type of BsAb activates the immune system at the tumor site.
- Cytokines: Abnormal regulation of cytokines is a key contributor in the development and progression of cancer, and research into BsAbs that may target two cytokines is largely still under way. One example is an agent that targets VEGF and ANGPT2, which are both involved in angiogenesis and tumor growth.
- Receptors: BsAbs can target two receptors on tumor cells allowing for inhibition of multiple pathways the cells use to grow and resist cancer treatments. An example is a BsAb that targets EGFR and cMET.
Nursing Considerations
BsAbs that engage the immune system can cause side effects commonly seen with immunotherapy agents, including a high risk for cytokine release syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS). For some BsAbs, the incidence of CRS in clinical trials was nearly 70%.
Nurses can use mitigation strategies to reduce a patient’s risk for severe CRS and ICANS:
- Premedication with a combination of antipyretics, antihistamines, or corticosteroids
- Step-up dosing schedules
- Hospital admission following administration for close monitoring, especially during early treatment cycles
Other common side effects include cytopenias, fatigue, musculoskeletal pain, and rash. Many BsAbs also have warnings for severe infection and embryo-fetal toxicity.
Administration varies widely and includes subcutaneous or IV routes, premedications, specific flushing practices, tubing requirement, post monitoring timeframe, and laboratory monitoring. At this time, some BsAbs are available only through a risk evaluation and mitigation strategy (REMS) program. Nurses should be familiar with the package insert for the drug they are administering and the requirements of any REMS program.
What’s Ahead
Several BsAbs are in clinical trials and may be approved in the next three to five years, and multispecific antibodies (e.g., trispecific, tetraspecific) are also in development. Oncology nurses can expect to see these agents more often and in a wide variety of cancer types, including possible approvals for solid tumor indications.
The complexity of administration, risk for serious side effects, and rapid evolution of indications and approvals can be overwhelming. Oncology nurses should engage the interprofessional team (e.g., pharmacy) and review agents’ package inserts or other relevant literature prior to administration to ensure they are well prepared to provide patient care.