For the past two years, patients and providers have turned their attention to combatting a global health threat. We’ve nearly crumbled amid the chaos, but carried on through acts of comfort and innovation. However, as we pled for an end to this nightmare, for heard immunity through vaccination, another health threat took a backseat. Cancer screening rates plummeted, particularly among communities of color. Oncology nurses can use evidence-based interventions to increase screening rates for all patients with cancer.
Acknowledging the Damage
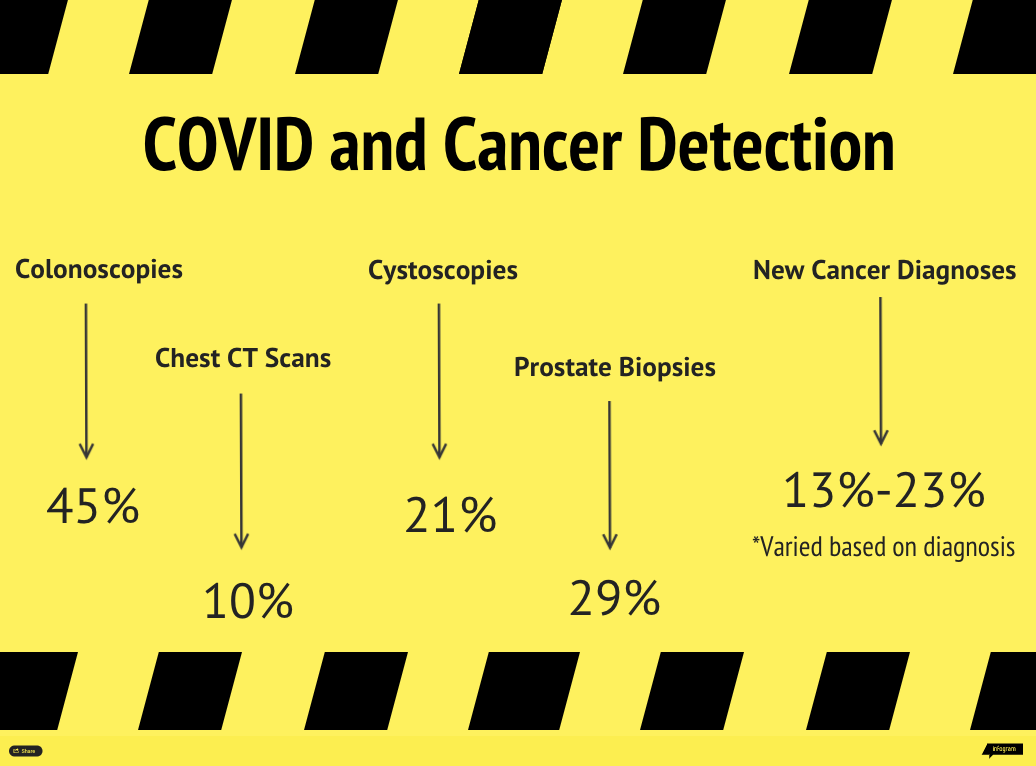
During pandemic, colonoscopies decreased by 45% in 2020 whereas prostate biopsies, chest computed tomography scans, and cystoscopies decreased by 29%, 10%, and 21%, respectively. New cancer diagnoses decreased by 13%–23% in 2020 compared to baseline years 2018 and 2019:
- 11,362 (23%) fewer prostate cancers
- 2,365 (13%) fewer lung cancers
- 2,130 (18%) fewer bladder cancers
- 1,979 (20%) fewer colorectal cancers
Bakouny et al. assessed the total number of screening tests completed during the:
- Three-month period immediately preceding the March 1–May 31, 2020, stay-at-home orders
- First three months of the pandemic in early 2020
- Same three-month period in 2019
- Three-month period immediately after the initial stay-at-home period
Based on information from Englum et al. (2021)
Interestingly, the researchers found that the percentage of positive results from a screening test increased during the pandemic when compared to the other time points, perhaps indicating a very diligent and judicious triaging effort to identify those most at risk. However, Bakouny et al. also reported that roughly 1,400 cancerous and precancerous lesion diagnoses were still missed that would’ve been caught if the same number of patients screened in the months leading up to the stay-at-home orders had been screened during the initial three months of the pandemic.
How to Respond
Reimagining how to target at-risk people for continued screening efforts was a priority and, even as the public followed stay-at-home orderes, researchers were actively exploring strategies to regain prepandemic screening rates.
The Population-Based Research to Optimize the Screening Process (PROSPR), a National Cancer Institute–supported consortium of healthcare systems across the United States, developed recommendations for improving cancer screening efforts, including home-based cancer screening tests like the fecal immunochemical test for colorectal cancer and evaluating emerging tests not yet approved for use.
Text message reminders and patient education interventions on family-focused communication also increased screening rates, particularly for patients of color.
Researchers also acknowledged that screening guidelines must consider more than just a patient’s age. Landy et al. created a risk model to augment guidelines and found that it eliminated screening disparities for most racial groups.
Implementing new approaches requires collaboration between various healthcare professionals, and nurses are vital at every step of the collective effort. Oncology nurses should be well-versed in cancer screening recommendations and use every opportunity to educate patients and ask about their screening adherence. Thorough chart reviews enable nurses to identify the most at-risk patients, communicate directly with patients to schedule or discuss results, and assist in patient navigation through the screening process.
ONS Voice has a topic tag dedicated to advancements in early cancer detection, and the American Cancer Society, National Cancer Institute, and Centers for Disease Control and Prevention offer an array of patient-centered resources on the importance of cancer screening.






