As the use of oral oncolytics has increased in cancer care, so has the amount of time oncology nurses spend educating and counseling patients and caregivers on their use. Studies have shown that although it’s challenging for nurses to carve out, the time is well spent. Providing and reinforcing accurate, detailed information about oral chemotherapy, in terms appropriate for patients and family caregivers, may promote patient safety, optimal dosing, and adherence to the treatment plan.
In their article in the October 2014 issue of the Clinical Journal of Oncology Nursing, Matthews and Caprera explained how they developed a reference tool that oncology nurses can use to educate and manage patients receiving oral chemotherapies.
Oncology Nurses’ Role in Patient Adherence to Oral Chemotherapy
Matthews and Caprera cited studies that show that providing nursing education when oral chemotherapies are prescribed increases the conversations and supportive relationships between patients and oncology nurse providers. When these are lacking, oral adherence suffers.
They surveyed about 200 oncology nurses participating in one of 17 educational in-service programs on the topic of challenges to oral adherence in oncology. Participants reported frustration, time constraints, and limited or no experience with oral therapies as obstacles to providing optimal care. As patient advocates, the nurses said they felt an obligation to provide patients and caregivers with sufficient understanding of their oral chemotherapies to achieve safe, unsupervised self-administration.
FIGURE 1. ONCOLOGY NURSES’ ROLE IN ORAL CHEMOTHERAPIES
- Review orders for accuracy.
- Discuss with patients how they took the drug during the last cycle and how it was tolerated.
- Mange any side effects.
- Clarify misinformation or administration errors.
- Establish that patients have the required prescriptions and procurement routines in place.
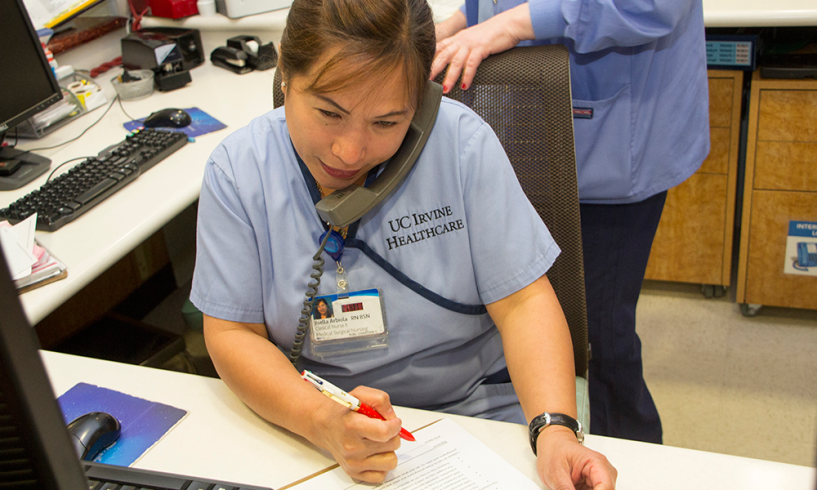
“When oral drugs are a component of cancer treatment, it adds another layer of responsibility for the oncology nurse,” Matthews and Caprera wrote. The nurse’s role is already complex (see Figure 1). Oral therapies require additional time for patient education, assessment, documentation, and follow-up. Oncology nurses also may spend more time on the phone with patients, pharmacies, insurance companies, precertification specialists, and other supportive agencies to help patients acquire and pay for their oral medications. Without useful tools to facilitate the workload, patient care may be compromised.
Creating a Tool to Monitor Oral Adherence
The authors praised the ONS Oral Adherence Toolkit for providing strategies and resources to facilitate adherence to 16 oral oncology drugs. “It contains easily accessible tools related to drug-drug interactions, administration directions (with or without food), safe handling, and common side effects. It includes useful information on assisting patients to overcome barriers to oral adherence, including emotional, psychosocial, and financial issues.” However, they noted that the toolkit doesn’t contain monitoring guidelines to follow patients while they are taking oral chemotherapies.
Nonadherence is a well-established problem in oral oncolytics. Matthews and Caprera pointed out that most oncology clinicians feel that they can safely assume that patients will adhere to their cancer treatments because of the seriousness of their diagnosis and the drugs’ critical role in treating their cancer. However, they noted that studies have shown that actual patient adherence to oral chemotherapies can be as low as 20%.
Essentials of Oral Oncolytics Guide
To help oncology nurses monitor and manage patient adherence to oral chemotherapy, the authors created the Essentials of Oral Oncolytics Guide (EOOG). “[It] provides useful information about currently available oral oncolytics (described as “targeted” or “novel”) in a simple format, focusing on and summarizing essential aspects of each drug,” Matthews and Caprera wrote.
The guide contains the following elements for each oncolytic covered.
- Indication(s)
- Recommended testing before starting and while monitoring patients receiving the drug
- Dosing and dose adjustments
- Adverse events or precautions
- Any black box warnings
They deliberately excluded hormonal agents (e.g., tamoxifen) and older oral chemotherapies (e.g., cyclophosphamide) to limit the number of agents covered and the size of the guide. “Keeping the information as abbreviated as possible makes the tool more useful, particularly for telephone triage,” the authors noted. Additionally, they intend to add to the guide as new oral agents are developed and approved.
For more information on the EOOG tool and to learn how oncology clinicians can receive a copy for clinical use, refer to the full article by Matthews and Caprera. The authors are seeking help in measuring and validating the tool and encouraged those who use it to report their experiences with it. To discuss oral adherence with other oncology nurses, join the ONS Oral Adherence Focus Group.
Additional Resources
- For more information on telephone triage, refer to Telephone Triage for Oncology Nurses.
- For more information on chemotherapy best practices, refer to Chemotherapy and Biotherapy Guidelines and Recommendations for Practice.
Five-Minute In-Service is a monthly feature that offers readers a concise recap of full-length articles published in the Clinical Journal of Oncology Nursing (CJON) or Oncology Nursing Forum. This edition summarizes “Essentials of Oral Oncolytics: Developing a Nursing Reference,” by Jennifer Matthews, RN, MSN, NP, OCN®, and Patricia Holland Caprera, RN, BSN, MBA, OCN®, which was featured in the October 2014 issue of CJON. Questions regarding the information presented in this Five-Minute In-Service should be directed to the CJON editor at CJONEditor@ons.org. Photocopying of this article for educational purposes and group discussion is permitted.