Switching from heparin to normal saline (NS) as the preferred flushing solution for central venous catheter (CVC) lines in adult ambulatory patients with cancer saved one institution nearly $30,000 without affecting quality of care, researchers reported in the Clinical Journal of Oncology Nursing. The change also increased patient safety by reducing risk of heparin-induced thrombocytopenia or allergic reactions, the authors said.
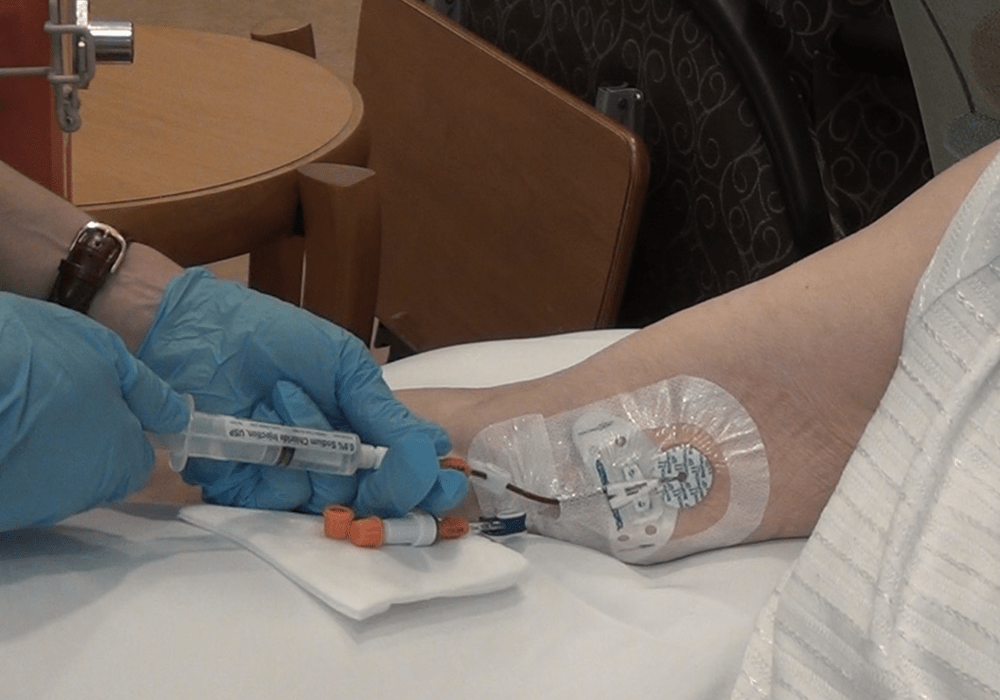
The study team, which included ONS member Phuong Huynh, MN, RN, OCN®, conducted a retrospective cohort comparison to “analyze the impact of preferentially using NS (versus heparin) flushes for CVC line maintenance for ports and other central lines (tunneled small- and large-bore CVCs, high-flow dual-lumen catheters) for patients with cancer.” They compared all adult patients who received care at their institution before (March 2019–March 2020) and after (March 2020–March 2021) implementing NS flushes.
The study intervention involved switching from heparin to NS as the standard for flushing and locking of CVCs in adult patients with cancer. They measured the impact on reported CVC line patency by the rate of tissue plasminogen activator (tPA) use, defined as administrations per line days. They also calculated cost data for NS versus heparin flushes and overall cost (including tPA) using the institution’s wholesale acquisition costs.
The researchers found that among the 3,706 active ports and 816 other central lines (high-flow dual-lumen catheters, tunneled small-bore CVCs, and large-bore CVCs) in the preintervention period, 294 patients with ports had at least one line occlusion and 78 patients with other central lines had at least one line occlusion. After implementing the shift to NS, among the 3,402 active ports and 694 other central lines, 460 patients with ports and 89 patients with other central lines had at least one occlusion.
They also found that tPA usage rate for ports increased from 1.05% preintervention to 1.59% postintervention (statistically significant) and for other central lines increased from 0.66% preintervention to 0.83% postintervention (not statistically significant). However, despite the increase in tPA usage rates, the estimated overall institution cost decreased by $28,696.
“This study demonstrated that NS flushes are as effective as heparin flushes for maintaining tunneled CVC and high-flow dual-lumen catheter patency in adult outpatients with cancer,” the authors concluded. “In addition, standardizing to NS flushes for CVC care is the safer option for patients in terms of routine heparin use increasing risk of complications, such as heparin-induced thrombocytopenia and patients with documented allergies unintentionally being flushed with heparin. Implementing NS flushes as the standard for CVC management also reduced overall cost to the institution.”
They recommended that future studies expand on their work by investigating NS flushes for other populations, such as pediatric patients undergoing transplantation, and for other line types.