During a patients’ initial visit, they’re asked to fill out a screening tool that helps provide a clearer picture as to what their home life is like. This tool addresses important information that helps to dictate our care. Though patients may feel like this is “just another piece of paperwork,” it is crucial to helping us understand their needs and to begin planning for special precautions we many need to take going forward.
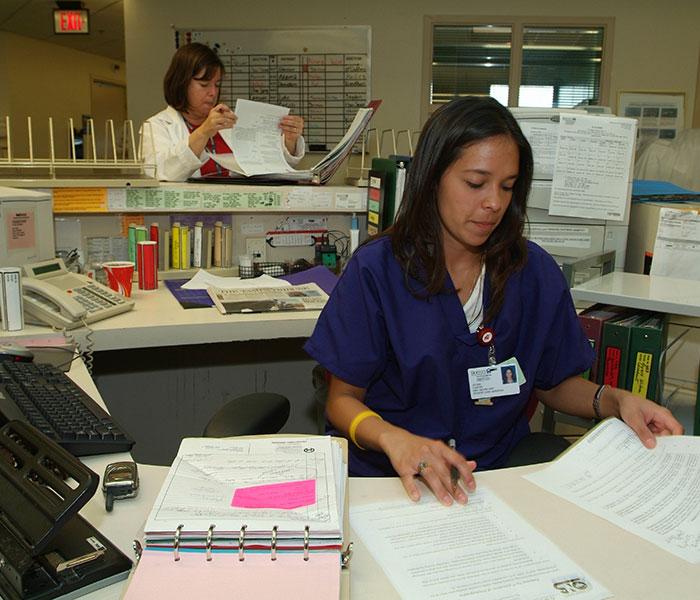
The “ambulatory health screening” encompasses factors such as allergies, implants (mediports, catheters, metal), infection control, assistive devices, nutrition, pain, tobacco screening, psychosocial distress, and finally the advance directive. Each one of these factors has a special way of keeping our patients safe. When the primary nurse reviews this document, she or he is required to input the information into the electronic medical record. From then on, referrals are generated based on the patient’s responses on the sheet. When this information is put into the system, the allergies, falls risk, and infection control fields are populated into an area in bold, colored fonts right next to the patients name and identifiers. These three prominent categories, at the very minimum, protect our patients and guide the healthcare team in making clinical decisions.
When I was working as a new nurse on an inpatient unit at Memorial Sloan Kettering (MSK), I was so busy keeping myself afloat and tending to the tasks at hand all while earnestly learning how to care for acute patients. Thanks to the ambulatory health screening, when my admission showed up her or his risk factors were already documented in the system. All of the identifiers that popped up on my screen, unbeknownst to me at the time, were filled out during the initial visit and revised over time by the patient’s primary nurse.
Sometimes during my inpatient shifts, I would receive patients with a clean slate—no factors flagged identifying them as a falls risk, on isolation precautions, or no known drug allergies. But as we know, these things change from shift to shift, patient visit to patient visit. When these details change, nurses update these factors in real time.
As any inpatient nurse can tell you, falls, drug reactions, and positive cultures can quickly turn your shift sour. If these events are documented properly, they can easily become a single instance that the patient and the clinical team can move forward from. These are events that help guide plans of care, and most importantly to help tweak plans in order to keep patients safe. In retrospect, it is very clear to me that the depth of our work is dedicated to keeping documentation up-to-date for the safety and well-being of the patient.
Through the continuum of care at MSK, clinicians make big decisions regarding the lives of our patients. Any nurse at MSK can attest that their safety is a prominent part of our culture. It, by and large, has a lot to do with documentation. The first source document, the ambulatory health screening, can be the most helpful reference point in understanding a patient’s home life and their needs going forward.