The explosion of telehealth transitioned many aspects of cancer care to patients and caregivers as home-based options. However, as with any shift in procedure, disconnecting their own pumps requires additional preparation and processes. Two oncology nurses share how they set up systems to support safe home care for pump disconnection.
Many institutions scrambled for strategies in response to the COVID-19 pandemic, but for ONS member Renee Yanke, ARNP, MN, AOCN®, oncology clinical nurse specialist at Kaiser Permanente Washington in Everett, WA, the idea began before. Her concept to allow patients to disconnect elastomeric pumps at home sparked during the fall 2019 Kaiser Permanente oncology conference, where she learned that Kaiser Permanente San Francisco’s oncology division had implemented it.
In May 2020, they started a pilot using the elastomeric pumps and teaching patients to learn to disconnect and flush their ports. “The pandemic made us all really consider ways to limit patients’ trips into our oncology clinics and infusion centers,” she said.
Across the United States, the outpatient medical oncology division at Morristown Medical Center in New Jersey was also developing a program using home-based pump disconnection to improve patient satisfaction. Previously, patients returned to the infusion clinic for a fast-track appointment, which led to some discontent, ONS member Amanda Sarafin, MSN, OCN®, oncology clinical education specialist at Hackensack University Medical Center in New Jersey, who worked at Morristown Medical Center at the time, explained. Implementing the program allowed patients to stay at home to disconnect their pumps and improved workflow at the outpatient centers by freeing up chairs and minimizing returns.
Start With Education
Yanke said that Kaiser Permanente Washington’s patients are taught the process of disconnecting during their first treatment cycle, then practice a return demonstration during their next visit. For the return demonstration, patients practice flushing, disconnecting, and disposing of the pump and supplies until they can confidentially and successfully demonstrate it.
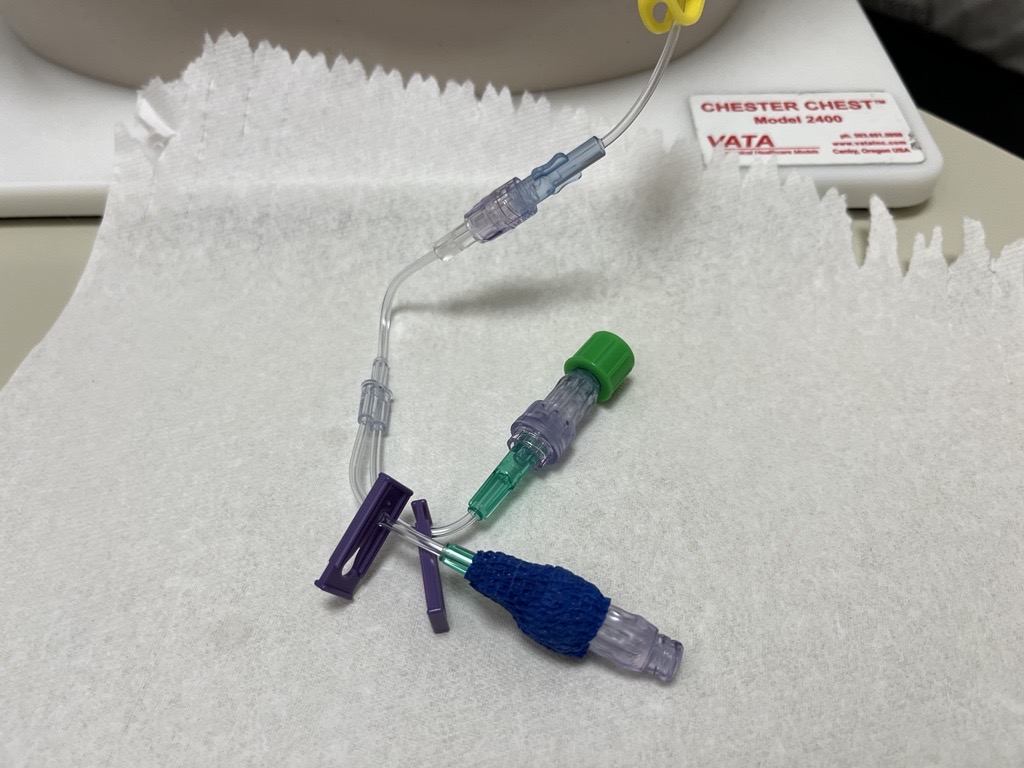
At both institutions, patients are sent home with all required equipment, including yellow chemotherapy bins, flushing supplies, alcohol wipes, gloves, and band-aids. They also receive reference handouts and guides on the process.
At Morristown Medical Center, Sarafin said the patient population selected was based on ability to learn safe handling of chemotherapy pump and the disconnection process. Nurses assigned to eligible patients assessed them for their willingness to disconnect their pumps at home. Participating patients then attend a nurse-led teaching session, which used a teach-back method where patients completed a hands-on demonstration.
At both institutions, handouts and visual guides were vital to educate patients and provide them with resources to follow at home. Yanke said that she and ONS member Catherine Jansen, PhD, RN, AOCNS®, oncology clinical nurse specialist at Kaiser Permanente San Francisco, collaborated to develop a patient handout that outlined the disconnecting process; specific steps such as reminders to clean the area, wash their hands, and gather supplies; and a phone number for the consulting nurse service.
Sarafin collaborated with a patient to ensure the handouts for Morristown’s step-by-step process were understandable. “I worked closely with a patient and her husband on making these directions clear and easy to follow,” Sarafin said. “This was super helpful!” Morristown also developed a tip sheet for patients to review when learning the process and later at home.
Another vital component of process implementation was educating the staff about explaining the process to patients and instructing them in safely flushing and deaccessing the implanted port at home. At Kaiser Permanente Washington, Yanke provided huddle cards that outlined a nurse’s role in the process, how to evaluate and teach eligible patients, connecting and disconnecting steps, patients’ supplies, and additional pointers. Yanke also shared information with urgent care and consulting nurse services during staff meetings and kept in contact with the pump manufacturer to have questions answered.
Morristown Medical Center instituted a hospital policy for specific details such as eligibility requirements and patient supplies. Furthermore, nurses received a presentation and a competency hour to review the training materials for proficiency. Some nurses, nicknamed “champs,” were tasked to keep the education and screening standardized.
Other general education included:
- Instructing patients and caregivers to check the pump’s decreasing in size, showing active infusion
- Instructing patients on the importance of and how to check the clamps
- Asking healthcare providers to support the process and encouraging patients to participate
Troubleshoot Challenges
Yanke had some questions about the elastomeric pump’s functioning and speed, which she was able to answer after consulting with the manufacturer. They also discovered that the PhaSeal closed-seal system transfer device for handling hazardous drugs often worked its way out of the connector and stopped infusing. To resolve the issue, Yanke said they dropped the use of the PhaSeal, taped the connection between the pump and the Huber needle tubing, and used the needle side port, which they capped for a clean injection and so the patient knew where to flush the catheter. After flushing, the syringe stays connected, and the pump, syringe, and tubing are all disposed of in the yellow chemo bin.
Patients were concerned about safely storing, handling, and disposing their chemotherapy at home, which led to a few patients opting out of home disconnection. Other patients needed several visits to feel comfortable performing the process themselves, Yanke said.
Sarafin said that meeting Morristown Medical Center’s approval process required solving a few key concerns. “The process needed to be approved by specific committees, along with the occupational safety team, because the hospital would allow the patient to return their bins once full and be provided with an empty one,” she explained. “Not to mention, the patient would be traveling in their car with trace chemotherapy and sharps. It was probably the biggest hurdle to get approval for.”
Analyze the Results
Three months into implementation, Yanke conducted pilot site outcome evaluation. Twenty-nine patients were recorded self-disconnecting their pumps at home for a total of 144 visits to the institution. The pilot site documented four infusion problems, with a 1.8% rate of problems and 98.2% success rate. During interviews, patients reported being satisfied with the pump’s light weight and small size for carrying.
“Within six months of starting, all five clinics began using the elastomeric pumps with success and happy patients,” Yanke said. “It would not have been successful without the nurses’ involvement. We continue to learn new things and are now standardizing a home spill kit and instructions for patients.”
Although Sarafin is no longer with Morristown Medical Center, outcomes were satisfactory during her time there. “Patients really valued and appreciated this implementation,” she said. “The process helped tremendously during the COVID-19 pandemic.”
Sarafin said that Morristown Medical Center extended the process to the rest of its campuses, increasing patient satisfaction and streamlining the practice across the system.






