When my mother died 10 years ago, I found an index card on which she had written a saying she titled “A High Calling.” It described parents’ important role in raising the next generation, their children. That message also applies to the preparation of the next generation of a profession, such as oncology nursing—beyond formal prelicensure education.
In my five decades as a nurse, I have heard many concerns about the preparation of each new generation of nurses. My generation was told that our training in nursing skills was too limited; thus, we could not fully function on day 1. That expectation most likely came from a history of nurses training in hospitals and quickly learning the practical, hands-on part of nursing. Today, I hear comments that new nurses don’t have skills with real patients because so much of their education was in simulation labs and that they want to advance too quickly in their careers. Internships, residencies, and academic partnerships are designed to bridge the gap, but the disconnection between academia and clinical practice remains and creates tension between generations of nurses.
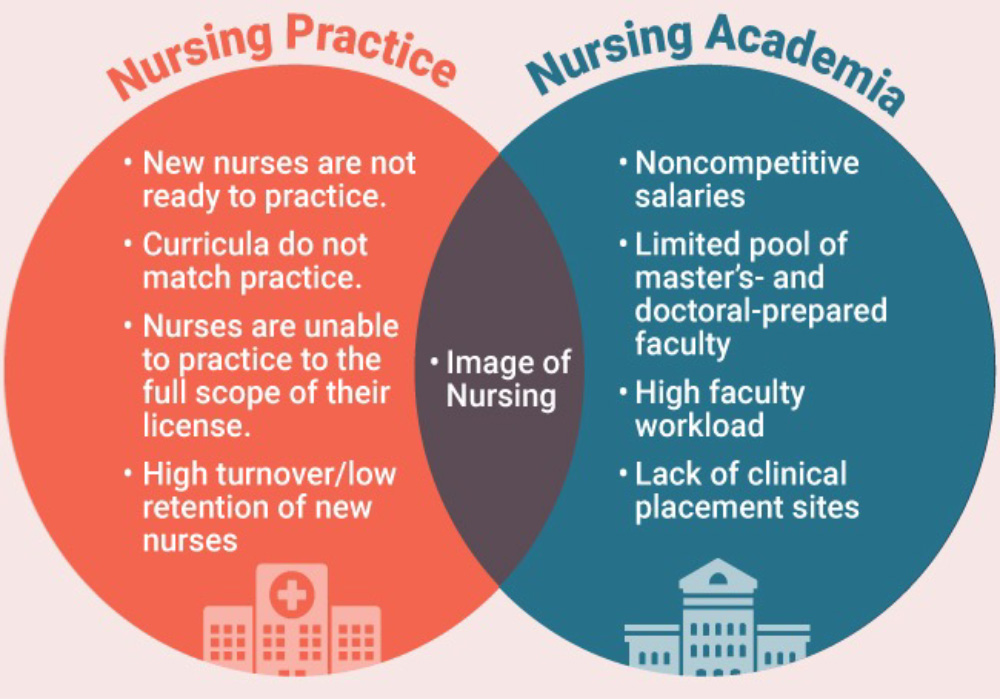
The American Association of Colleges of Nursing (AACN) and American Organization for Nursing Leadership (AONL) summarized the challenges that the academic and practice settings both face during a 2023 joint meeting (see sidebar for a few of the primary issues).
I read an interesting perspective on how words can influence the perception of our profession, particularly how they reinforce a hierarchical health system. The author wrote that terms such as staff nurse, floor nurse, bedside nurse, or clinic nurse do not portray a nurse’s expertise and authority. She contrasted the terms used for nurses to those used for physicians, such as hospitalist and intensivist, or by the specialty, such as oncologist. The phrase, “just a nurse,” has always bothered me, especially when a nurse uses it. Beginning with prelicensure education, nurses need to be deliberate about the language they use. Does it convey your professional expertise, authority, and autonomy?
No single solution will meet the challenges that AACN and AONL identified or close the academic–practice gap. However, each of us can be mindful of what we say when we talk about being a nurse and how we support new nurses. One strategy AACN and AONL mentioned in the report is to encourage students to be bold and courageous, to challenge the status quo. That may mean that those of us who created the current structures, norms, and behaviors have to be willing to change.
Certainly, paying attention to the language we use is a start. A good place to begin is using phrases like, “My education, training, and experience help me provide you with the best care,” rather than, “I’m just doing my job,” when patients show appreciation. Another is to embrace the generational transfer of wisdom and expertise, giving generously and receiving respectfully.






