Focusing on a patient’s quality of life is often a key component to their successful cancer journey. Treating their disease is crucial, but patients have to be recognized as individuals with unique and varying needs. Addressing their emotional, physical, spiritual, and psychosocial stressors can help provide holistic treatment that’s at the heart of successful oncology care.
Supportive care programs—which include everything from palliative care to therapeutic music, meditation, yoga, exercise, and counseling—aim to decrease patient burdens and improve quality of life by addressing tangible and intangible elements of patient-centered care. Connecting patients with available supportive care resources can better manage symptoms, reduce distress, and improve their overall quality of life.
What Supportive Care Programs Entail
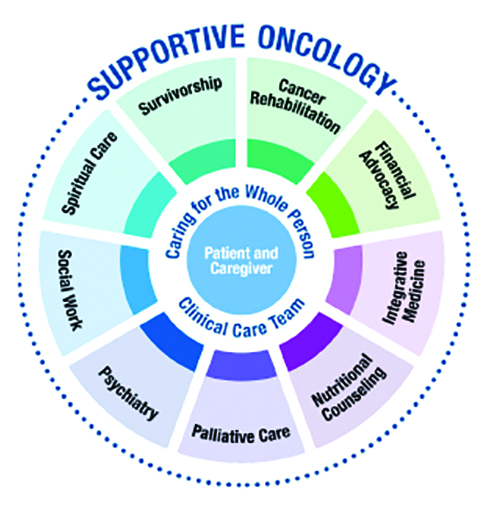
For many healthcare professionals, supportive care programs might conjure ideas of complementary treatments or integrative medicine, but that’s just one part of the whole supportive care picture. As a group, the programs, resources, and advocates help patients address the multifaceted issues that come as part of a cancer diagnosis.
“Supportive oncology is a large, coordinated framework that includes a number of resources for our patients,” ONS member Linda Penwarden, MN, RN, AOCN®, clinical nurse specialist at St. Luke’s Mountain State Tumor Institute in Boise, ID, says. “Our programs and resources include rehabilitation, financial advocates, access to multidisciplinary experts, and integrative medicine, including acupuncture, massage, and strength and conditioning. We also have oncology dieticians, psychiatric care, social workers, chaplains, and a robust palliative care program—which is an entire field unto its own and includes many of these programs and more under its own umbrella. We hold survivorship clinics and provide care plans for our patients.”

Supportive care takes many different shapes in practice. ONS member Vivian Sarubbi, RN, PHN, BSN, a charge nurse at Pacific Cancer Care and Community Hospital in Monterey, CA, serves dual roles for her patients—she’s a nurse and a certified clinical musician. She provides therapeutic music to a wide spectrum of patients as they navigate their cancer journey.
“Therapeutic music has been proven to show major benefit to patients, healthcare staff, and family members,” Sarubbi explains. “A national standards board reviews certification programs for therapeutic musicians, and advanced training is involved. Different music and tones have been shown to be effective for different patients and situations. The goal is to provide a cradle of sound to comfort each person.”

Sarubbi looks at the music she plays as a sonic massage, and she notes the importance of reading her environment and patient moods. Her harp therapy program offers comfort, reduces anxiety, regulates heart rate, increases oxygen saturation, slows respiration, and helps patients rest and relax. Sarubbi also mentions its effectiveness as a sleep aid.
“Some of my patients can fall into a deep rest and sleep after I play for them,” Sarubbi says. “Sometimes I’m shocked at how quickly it can help them sleep. Most patients struggle getting sleep in a hospital, and they’ll comment saying how easy it was for them to relax. It really helps transport them to a different place and time.”
The Benefits of Supportive Care Programs
Both Penwarden and Sarubbi have seen their patients embrace supportive care programs, including music, meditation, yoga, exercise, and writing therapy, depending on their individual needs.
“Our philosophy is about caring for the whole person, not just the disease,” Penwarden says. “When I circle back with patients during treatment, they really express how beneficial some of these programs are. They’ll tell me, ‘So-and-so really helped me figure out my insurance,’ or some of our head and neck patients will meet with dieticians and comment on how important and beneficial that was for them.”
Sarubbi says she’s witnessed patients respond in different ways and require different things from the therapeutic music she provides.
“For dying patients, the music can provide a calming effect, bring them emotional well-being and a sense of peace,” Sarubbi says. “Music can help patients with memory impairment or chemo brain awaken their sense of the present and help with memory recall. In fact, there’s a documentary called Alive Inside that I recommend to healthcare providers that shows the power of music on patients with different types of illness.”
Additionally, by meeting patient needs in other ways, supportive care programs can free up time for oncology nurses to focus on other pressing aspects of their patients’ care.
“If patients are experiencing emotional distress and they’re not seeing the chaplain or social worker, it can be a benefit all around to refer them to the expert,” Penwarden says. “Not only does that connect them with someone who deals with these issues all the time, it also allows nurse to spend more taking asking questions about their physical condition. When you look at the resources available and refer patients appropriately, everybody wins.”
Barriers to Supportive Care Programs
Penwarden cites time as a factor in supportive oncology care. Finding the opportunity to broach the subject with patients can be difficult among all the other important tasks involved with care for patients.
“As a nurse, you’re trying to start the IV, get the antiemetics in, start the chemo, and it’s hard to stop and have time to revisit other aspects of supporting your patients,” she says.
Sarubbi says that some people associate her instrument with mental images of the end-of-life experience or angels playing harps. She works to overcome those misconceptions by explaining the benefits of therapeutic music and how it can improve their well-being.
“Sometimes I’ll get a raised eyebrow,” Sarubbi says. “I just ask them, ‘Would you like to try it out?’ When we do, they’re often surprised by the benefits. They’ll say to me, ‘Oh my, I had no idea. The music relaxed my body and the stress just fell away.’ In fact, harp therapy has been around since ancient Babylonia. It’s been shown to be effective at all stages of health from birth through physical illness and into the end of life. It’s all about playing to the needs of the patient.”
Integrating Supportive Care Into Practice
Linking patients to the right supportive care program might seem difficult. Sometimes patients aren’t sure of the benefits or may not see an immediate need for supportive care. For Sarubbi, it’s about providing them with options.
“I always tell them to choose and explore from the smorgasbord of resources that would help them best,” Sarubbi says. “I encourage them to try different types of therapeutic music, acupuncture, journaling, art therapy, nature walks, massage, therapy animals, energy work, and any of the other things available. Give them choices, because patients often forget what’s out there.”
Penwarden’s institution offers introductory education—along with regular reminders—to help outline options for patients.
“Since 1999, we’ve been inviting new patients to a class called TLC, which stands for Treatment Learning Class,” Penwarden says. “It’s one place where we introduce our supportive oncology services. Patients will get their diagnosis, see their provider, determine a treatment plan, and attend our TLC program. It helps outline all of the programs we have at St. Luke’s that fall under the umbrella of supportive oncology. Because the beginning of treatment can be overwhelming with new information, we also have TVs in all our lobbies and waiting rooms that have our supportive oncology services listed. That way patients and families are reminded of the services throughout treatment.”
With the abundant programs and emerging opportunities for further research, supportive care is making its way into everyday practice.
“Some supportive care programs might not be for everyone and that’s okay,” Penwarden says. “But I do think it’s time for insurance companies to step up and cover as many of these programs as possible. Real people benefit from supportive oncology programs. For some, it really helps get them through their treatment.”
Ultimately, holistically supporting patients through their treatment can make an enormous difference in their quality of life and emotional and physical well-being.
“Supportive care is a necessary addition for patients undergoing treatment. It can be incorporated from a patient’s diagnosis onward,” Sarubbi says. “Programs like harp therapy and resources like acupuncture, mindfulness, and more can help heal the mind, body, and soul of patients with cancer. It impacts the individual person, and it highlights the humanity of our care.”