The relationship between nutrition and cancer outcomes is complex. Nutritional status is closely linked to cancer treatment outcomes as well as the prevalence and tolerance of side effects. Oncology nurses often educate patients about proper nutrition throughout their cancer journey, but adherence requires patients to have access to nutritious food.
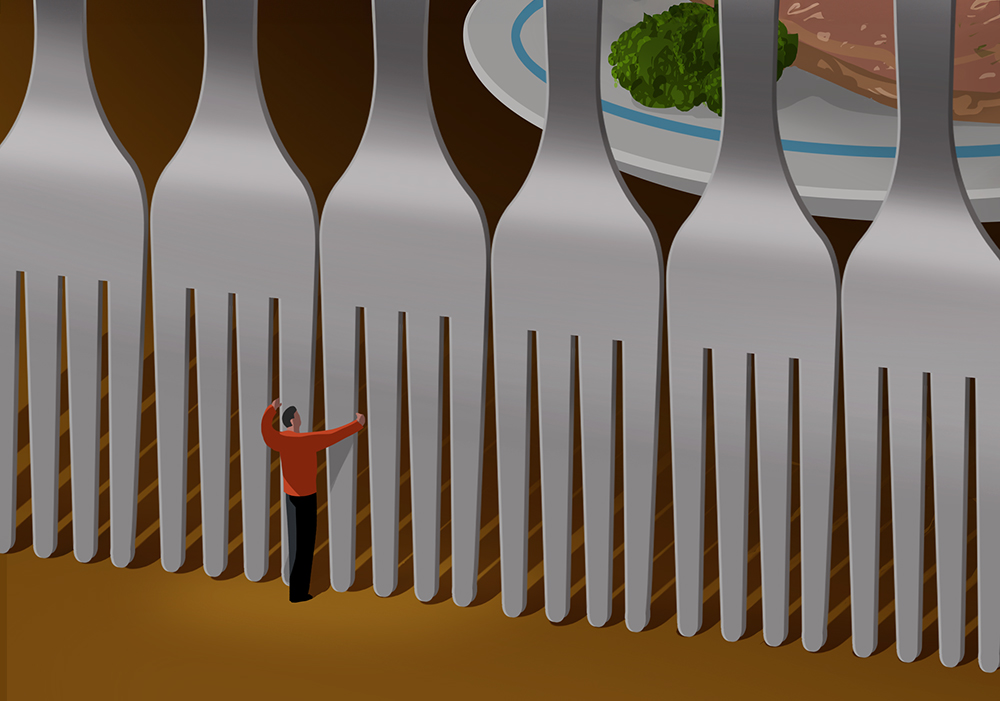
Food insecurity, or “household-level economic and social condition of limited or uncertain access to adequate food,” has been rising in the United States, according to the U.S. Department of Agriculture. In 2022, an estimated 12.8% of U.S. households were food insecure, a 25% increase from 2021’s 10.2% in just one year. However, the statistics are even higher for patients with cancer, ranging from 17%–55%. The cancer-related increase is associated with many factors, including costs of care, inability to work, and other financial toxicities of cancer treatment.
“Food insecurity is a spectrum of uncertainty or limited access to food, impacting diet quality, variety, and other factors that disrupt eating patterns and can lead to hunger,” Mariah K. Jackson, PhD, RDN, LMNT, said. Jackson is an assistant professor of the medical nutrition program in the department of medical sciences at the University of Nebraska Medical Center in Omaha who copresented a 2024 ONS Congress® session, Tackling Nutritional Barriers in Vulnerable Populations: Practical Solutions, with Caitlin Benda, MBA, MS, RD, CSO, a registered dietitian and board-certified specialist in oncology nutrition at Inova Schar Cancer Institute and Life with Cancer in Fairfax, VA. Jackson and Benda provided specific information on the impact of nutrition, as well as screening and mitigation tips.

Nutrition Is Even More Important During Cancer Treatment
“During cancer treatment, protein and calorie needs are often higher, and dietary advice must be tailored to focus on symptom management, like decreased appetite, taste changes, and nausea,” Jackson advised.
For example, patients preparing for surgery or treatment should eat high-protein foods, including plant-based proteins like beans, lentils, quinoa, soybeans, nuts, and tofu. Patients who eat meat and dairy can get protein from sources like cottage cheese, lean meats, eggs, and Greek yogurt.
During treatment, side effects such as nausea and vomiting, dysgeusia, xerostomia, mucositis, diarrhea, and constipation can result in nutritional insufficiencies in even the most food-secure patients that may affect treatment outcomes, survival, and quality of life. Malnutrition also lowers functional status and prolongs recovery times.
“Combining nutritional vulnerabilities with food insecurity creates an even higher risk for malnutrition,” Jackson said. She said that food insecurity is also associated with lower treatment adherence, because patients who are food insecure are more likely forgo, delay, or make treatment changes than food-secure survivors. Therefore, patient interactions should focus on effective screening and identifying—and taking action on—food insecurity to improve patient outcomes.
“Food insecurity should be targeted to help remove a layer of malnutrition risk in this highly vulnerable population,” Jackson said.

Food Insecurity Is Often Hidden
Because of shame, embarrassment, or fear of being judged, patients may hide their nutritional struggles. However, nurses can use screening tools, such as the Hunger Vital Sign validated two-question screening tool, or ask simple questions and observe for signs of malnutrition, even if patients downplay their symptoms or try to avoid discussing their dietary habits.
Benda advised nurses to watch for signs that a patient may be struggling with food insecurity, such as hoarding or stockpiling food offered in the infusion clinic or frequent reports of skipping meals. She added that mobility issues and lack of access to transportation or the Internet may also influence a patient’s ability to access healthy food, appointments, and knowledge. She also reminded nurses that malnutrition doesn’t necessarily equate to body size.
“Patients who appear well-nourished or of healthy weight may also be misidentified as not being at risk for nutrition issues, but nutritional deficiencies and food insecurity can affect individuals of all body sizes,” Benda said. “Like all individuals, nurses can hold hidden or implicit biases that may influence their perception and management of food insecurity or malnutrition in patients.”
Potential biases include:
- Weight bias occurs when healthcare professionals consider malnutrition only in patients who are underweight or visibly malnourished, which could lead nurses to overlook or underestimate malnutrition in individuals who are experiencing overweight or obesity, as well as food insecurity.
- Health literacy bias occurs if healthcare professionals think that patients with higher health literacy or education levels are unlikely to have food insecurity or nutritional challenges.
- Language, communication, and culture biases could lead healthcare professionals to misunderstand or misinterpret patients’ nutritional concerns. Biases may also relate to a patient’s cultural beliefs or practices related to food and nutrition, which could impact healthcare professionals’ understanding and assessment of a patient’s nutritional status or access to food.
For patients with risk for or suspected malnutrition, Benda and Jackson said that fat loss can be assessed in subcutaneous locations (orbital fat pads, buccal fat, triceps, and ribs), upper-body muscle fat locations (temples, clavicle, shoulder, scapula, and hands), and lower-body muscle fat locations (thighs and calves). Fluid accumulation, which can be associated with congestive heart failure and kidney or liver disease, is assessed by touching the top of the foot, ankle, and tibia bilaterally to observe pitting. See ONS Voice’s “8 Ways to Help Your Patients During Hunger Action Month” for more information on screening and examination resources.
The Integral Role of Oncology Nurses
Oncology nurses have several ways to support patients experiencing food insecurity, Benda said:
- Early identification of nutrition-related problems: Nurses can help patients overcome nutritional challenges during cancer treatments through early identification and treatment of nutrition-related problems, starting with regular nutritional assessments and screenings.
- Early education and counseling: Nurses can help patients and families understand the importance of maintaining nutrition during cancer treatments and managing treatment-related side effects to allow for adequate intake.
- Close collaboration with registered dietitians: Dietitians can develop individualized nutrition plans based on patients’ specific needs, treatment regimens, and dietary preferences. Oncology dietitians can provide expert guidance on optimizing nutrition to support cancer treatment outcomes and overall health.
- Coordinating care among the healthcare team: Nurses who identify patients with food insecurity can make referrals to social workers, community resources, and support services.
Oncology nurses can make a difference by advocating directly for individual patients, raising awareness among the cancer care team about the prevalence and impact of food insecurity among patients with cancer, and creating or supporting community partnerships with food banks, organizations, and nonprofits, Benda said. She recommended Feeding America, the Supplemental Nutrition Assistance Program, and local food assistance programs such as Meals on Wheels and community food pantries. Find other ideas to support your patients in ONS Voice’s “8 Ways to Help Your Patients During Hunger Action Month.”
Finally, Benda encouraged nurses to advocate for and collaborate on organizational initiatives, such as creating a food pantry in their cancer center, a concept that’s growing throughout the United States. Read about one example at the Mary Bird Perkins Cancer Center in ONS Voice’s companion article.