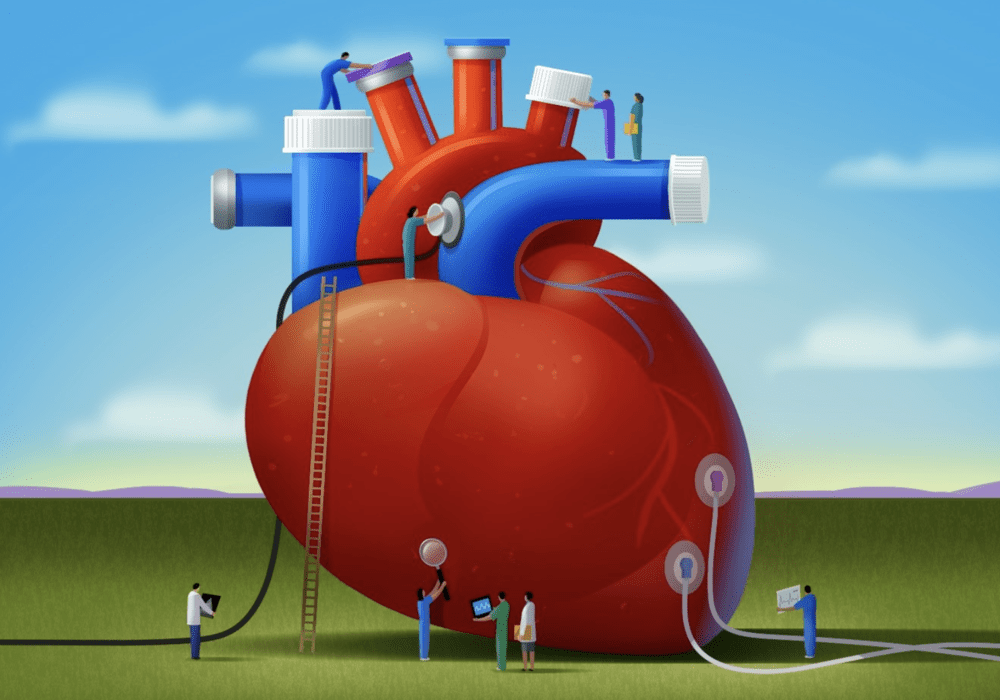
More than two-thirds of cancer survivors are aged 65 or older, which is often when the general risk for heart disease increases. Some cancer drugs increase patients’ risk for cardiovascular (CV) adverse events, such as arrhythmias, myocardial ischemia, hypertension, myocarditis, heart failure, and other cardiac complications. Here’s how oncology advanced practice providers (APPs) can assess for risk factors, implement prevention strategies (see sidebar), and improve the complex, coordinated care of patients receiving cardiotoxic drugs throughout the cancer continuum.
Learn the Latest in Cardio-Oncology
Begin by educating yourself and your oncology nurse colleagues at all levels of practice with resources from ONS and other professional organizations on preventing, mitigating, and monitoring cardiac toxicity before, during, and after cancer treatment (see sidebar). As part of that process, you may need to learn about new cardiac imaging tests and understand how the results are reported.
Echocardiography is the mainstay to evaluate left ventricular ejection fraction in patients with cancer. Emerging studies are testing assessment of global longitudinal strain (GLS) using speckle tracking echocardiography to detect and quantify early subtle disturbances in global long-axis left ventricular systolic function. A relative GLS decrease of more than 15% from baseline during cancer treatment is considered cardiac dysfunction. Several guidelines also recommend using cardiac biomarkers, such as troponins and natriuretic peptide, to monitor for cardiac dysfunction.
Incorporate Guidelines in Practice
Several drug classes are known to cause cardiotoxicity, some with higher risks than others. Patients receiving anthracyclines, HER-2 monoclonal antibodies, vascular endothelial growth factor inhibitors, proteasome inhibitors, and tyrosine kinase inhibitors are at higher risk for developing cardiotoxicity when combined with other risk factors, such as chest radiotherapy, age 60 or older, preexisting heart disease, elevated baseline cardiac biomarkers, and other chronic illnesses (e.g., diabetes mellitus, hypertension, obesity, tobacco use, dyslipidemia, chronic renal insufficiency). In addition, several immunotherapies (e.g., checkpoint inhibitors, immunomodulatory drugs) and androgen-deprivation therapies also have CV risks and complications.
Determine Disparities
As part of routine assessment of social determinants of health (SDOH) for all patients with cancer, APPs should give special attention to Black patients with breast cancer because of their higher risk for CV events and cardiotoxicity with an earlier onset that may be influenced by SDOH. Factors such as financial, housing, or food insecurities; lack of access to transportation; and racial discrimination may reduce those patients’ ability to practice lifestyle behaviors that patients without barriers could use to reduce their risk for CV disease and treatment-related cardiotoxicities. Oncology APPs can use their role to advocate for patients and collaborate with community providers to address individual needs and connect patients to appropriate services.
Contribute to Program Development
Oncology APPs are in a pivotal position to monitor for cardiotoxicity, make early referrals to cardio-oncology clinics, and contribute to developing or improving cardio-oncology programs for palliative and survivorship care. Consider developing cardio-oncology registries to identify care gaps for patients with cancer, including adolescent and young adult survivors, or embedding risk calculators in electronic health records to support artificial intelligence–based risk assessment, cardiac risk stratification, cardio-oncology referrals, and early intervention. Clinical studies are also under way to investigate preventive strategies for cardiotoxicity.