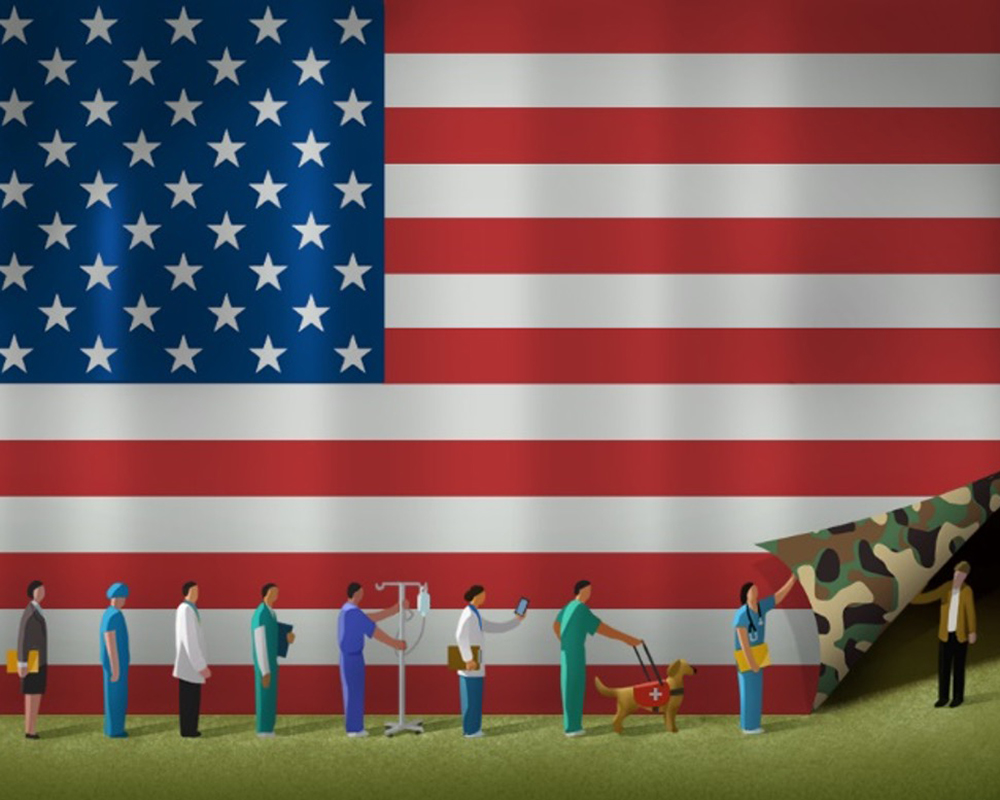
Veterans and active service members of the U.S. armed forces have dedicated their lives to the safety and freedom of their country. However, that honorable service may place them at risk for post-traumatic stress disorder (PTSD), anxiety, depression, and cancer.

According to the U.S. Department of Veterans Affairs (VA), more than 43,000 veterans have a new cancer diagnosis each year—16% of which are rare cancers—and more than 450,000 veterans are receiving cancer care at a VA hospital or institution. Cancer screening, testing, and treatment are critical for the veteran patient population. Whether they’re conducting research on the patient population or building supportive care programs, oncology nurses must weigh the unique care considerations and recruit the best resources for each individual veteran’s intricate background.
For Our Freedom, Service Members Face Cancer Risks and Challenges
“Veterans and active service members of the U.S. armed forces may have been exposed to different chemicals or environments that place them at a higher risk for certain types of cancer,” ONS member Mary Jane Willard, PhD, MBA, MA, RN, CCRN, clinical assistant instructor at the University of Arkansas for Medical Sciences (UAMS) in Little Rock and member of the Little Rock ONS Chapter, said. Willard cited a 2023 phase I study of cancer incidence and mortality rate among military aviators and aviation support personnel in which the researchers concluded that active service members or veterans may have varying increases in their cancer risk.
Among aviators and aviator support personnel from the Air Force (70.6% and 47.8%, respectively) and Navy (21.2% and 38.3%, respectively), researchers found that compared to the general population and adjusting for age, sex, and race:
- Air crew members had increased rates of:
- Melanoma: 87%
- Thyroid cancer: 39%
- Prostate cancer: 16%
- All cancers: 24%
- Ground crew members had increased rates of:
- Brain and nervous system cancers: 19%
- Thyroid cancer: 15%
- Melanoma: 9%
- Kidney and renal or pelvis cancer: 9%
- All cancers: 3%
Veterans also face specific challenges and barriers to accessing cancer care, with location being the biggest factor. More than half of veterans in the VA system live in rural or very rural areas, but 66% of rural U.S. counties have no oncologist.

“Patients may have long commutes to a healthcare facility for appointments and treatments, and many veterans need reliable transportation and funds to cover fuel,” Donna McCallie, RN, MSN, OCN®, outpatient oncology infusion nurse in the cancer center at West Palm Beach VA Medical Center in Florida and member of the Palm Beach Area ONS Chapter, said. “Many in our veteran patient population have mobility issues because of injuries or illnesses, so they use motorized scooters, wheelchairs, or rolling walkers to get around. Some rely on special mode transportation, and even if a veteran is eligible for it, the service may be booked with no available openings when needed.”
Addressing Electronic Cigarette Usage Among Veterans
Social determinants of health affect many patients with cancer, but Willard’s research centers on factors associated with military members’ use of electronic cigarettes. She explained that although the evidence shows that tobacco cigarettes are associated with an increased risk of cancer, long-term data are not yet available for any connection between e-cigarettes and cancer.
“Despite the concept of a ‘healthy soldier effect’ that suggests that military members are healthier than the general population based on the military’s vigorous fitness requirements,” Willard said, “military members and veterans are more likely to use tobacco products.”
Among the military branches, the U.S. Marine Corps has the highest rate of smoking tobacco cigarettes (30.8%), followed by the Army (26.7%), Navy (24.4%), Coast Guard (19.9%), and Air Force (16.7%). The U.S. Marine Corps also has the highest rate of e-cigarette use (16.2%), followed by the Navy (14.5), Army (11.2%), Air Force (10.5%), and Coast Guard (9.3%). In a 2015 Department of Defense survey, 49.2% of active-duty service members reported using a nicotine product in the last 12 months and 62% of the entire VA population smoked tobacco cigarettes.
In 2022, Willard conducted a cross-sectional, correlational study that included military members aged 18 and older using the Behavioral Risk Factor Surveillance System and military-related questions and found that “military members reported higher usage of both e-cigarettes and tobacco cigarettes than previously reported in the literature.” Of the 434 participants, 223 reported dual use (tobacco cigarettes and e-cigarette use combined), 67 used only tobacco cigarettes, 37 used only e-cigarettes, and 107 were nonusers.
Willard also found a statistically significant association between stress and depression and dual use and nonuse. “Several psychosocial factors may contribute to dual use in the military,” she said. “Helping with concentration, stress, depression, decrease anxiety, and reducing appetite were all reasons for using e-cigarettes or dual use. Military members may be self-medicating with nicotine, leading to a much greater problem.”
When Willard presented her findings to her local ONS chapter, she discovered that many oncology nurses had not received any formal training on e-cigarettes and their associated safety concerns. She called for more oncology nursing education on the topic and encouraged her nursing colleagues to consider each individual patient and their home environment, education level, personal healthcare resources, health-related community resources, and resources needed upon discharge, including referral to smoking reduction or cessation programs when necessary, to address any social determinants of health.
Service Dogs Support Those Who’ve Served
Various strategies offer military members and veterans a healthier alternative to tobacco or e-cigarettes to manage their psychosocial well-being, such as the support of an animal companion. In 2014, the VA began the first randomized controlled trial to evaluate whether service dogs could provide therapeutic and economic benefits for veterans with PTSD. It compared the effect of service dogs and emotional support dogs on overall functioning and quality of life, mental health outcomes, healthcare costs, and employment and productivity. The VA found that animal-assisted therapy had positive results, and the idea to create programs to pair service animals with veterans began to snowball.
“A cancer diagnosis is a significant stressor for anyone who does not have PTSD,” McCallie said. “Veterans who have been diagnosed with PTSD then have additional life stressors added to them and their families, such as financial burdens, emotional drain, scheduling conflicts, and relationship strain. Depression often accompanies PTSD, which can be compounded by the additional stress of a cancer diagnosis and interfere with effective coping mechanisms.”
McCallie’s institution is one of five selected VA facilities nationwide that participates in the Puppies Assisting Wounded Servicemembers (PAWS) pilot program. Through PAWS, veterans with PTSD help train service dogs for other veterans in the community, which may in turn increase the participating veteran’s sense of purpose and self-worth by helping other veterans. In May 2023, the West Palm Beach VA Medical Center graduated its second cohort.
One of McCallie’s patients always brought his service dog—a golden retriever—to his treatment visits at her cancer center. The veteran’s cancer treatment plan also involved an inpatient surgical procedure at the facility, but he could not find anyone to care for his service dog during his admission.
“I was stunned to learn that the surgeon who performed the procedure took his patient’s service dog into his own home to care for him that evening,” McCallie said. “When I saw the surgeon a few weeks later, I thanked him for taking care of the dog. The surgeon replied, ‘Are you kidding? It was my treat. The dog slept in my bed with me. It was great!’”
Facilitate High-Quality Cancer Care Through Communication and Research
Although oncology nurse and other scientists have uncovered the social determinants of health and barriers to care that veterans with cancer face, they must dig deeper, Willard said. Direct care nurses can use that evidence to develop and promote resources to help military members navigate a cancer diagnosis and treatment.
Open communication with each of your patients helps you identify their individual barriers and concerns and develop a plan to address them, Willard said, and it extends to the interprofessional care team as well. For example, she said that her team actively participates in interprofessional rounds to identify and address goals and barriers to care early in a patient’s admission. Because of her research and clinical focus, smoking cessation programs are often involved.
“My best tip is to remember that veterans are just people who happen to have cancer, too,” McCallie said. “Like all of my patients, I try to get to know them and make them feel comfortable, valued, and appreciated. That is the human element that oncology nurses provide every day, no matter their role.”