Building Collaboration, Education With Oncology Nurses in Malawi
Nestled between Tanzania and Mozambique in eastern Africa, Malawi is a country of more than 18 million citizens. It faces a unique cancer burden that’s proven challenging for practitioners and patients alike. With a high prevalence of HIV-infected individuals, Malawi sees a proportionate rate of AIDS-related cancers (http://malawicancerconsortium.web.unc.edu/home-page/background-and-significance/), including Kaposi sarcoma, cervical cancer, and non-Hodgkin lymphoma. Currently, healthcare professionals in the country face a lack of standardized oncology education and resources. Roughly 84% of the country’s citizens live in rural areas (http://malawicancerconsortium.web.unc.edu/home-page/background-and-significance/) with limited access to healthcare institutions.
To collaborate with local educators and oncology professionals to perform a comprehensive needs assessment, ONS member and Leadership Development Committee chair, Ashley Leak Bryant, PhD, RN-BC, OCN®, assistant professor at the University of North Carolina at Chapel Hill (UNC-CH) School of Nursing, ONS member Lixin Song, PhD RN, FAAN, associate professor and Beerstecher-Blackwell Distinguished Term Scholar at UNC-CH School of Nursing, and Nilda Peragallo Montano, DrPH, RN, FAAN, dean at UNC-CH School of Nursing, visited Malawi’s capital city, Lilongwe, from December 1–8, 2018. The assessment established the current status of oncology nursing education, research, and patient care in Malawi and identified areas where international support and global collaboration could grow.
Identifying Areas for Collaboration
Working alongside oncology professionals from the Kamuzu Central Hospital (KCH), Kamuzu College of Nursing (KCN), Malawi Palliative Care, and the Malawi Ministry of Health, Bryant, Song, and the team sought to learn more about the healthcare system throughout the country.
“My experience with oncology nursing and cancer care in the United States has been that patients are usually on an established time schedule. They come into the clinic, get blood work, see the nurse, see the oncology provider, and may get treatment or be transferred to the inpatient oncology unit,” Bryant said. “Malawi’s healthcare system is a departure from U.S.-based institutions. Patients are told to arrive on a certain day. However, depending on order of arrival, workflow, and staffing, they may or may not be seen by a nurse or oncologist. There aren’t any guarantees.”
Staffing issues were also highlighted as one of the obstacles that healthcare professionals face throughout Malawi.
“The patient-to-nurse ratios were extremely high—even in one of the best hospitals,” Song said. “We saw rates that had one nurse responsible for as many as 80 patients. The nurses also work extremely long shifts. For example, in one of the best hospitals, the day shift for nurses is from 7:30 am–4:30pm and the night shift is from 4 pm–8 am. That was something surprising that I learned from our visit. But we were also impressed by the devotion of these nurses, despite their lack of resources and support.”
As the nurses in both countries worked together, the team discovered areas for international collaboration that could further oncology nursing education, practice, and research in Malawi.
“We identified a few distinct needs, mainly related to education and interest in oncology nursing,” Bryant said. “Building the nurse’s clinical capacity by integrating content about cancer care into their nursing curriculum—which they don’t currently have—is vital. These nurses are hungry for that information. They’re aware of the global cancer burden, but they lack the oncology experts and resources to allow them to teach that content to students. Furthermore, we found common misconceptions about cancer care, like it’s only about treatment, side effects, and those who are dying.”
For many nursing students, Bryant said that stigmas and myths about oncology are driving them away from careers in cancer care. However, after the U.S. delegation had an educational oncology curriculum information session detailing the cancer continuum from diagnosis through treatment, survivorship, and into end-of-life care, nursing students at KCN recognized that cancer care is more than just harsh chemotherapy treatments and debilitating side effects.
Song also identified the lack of safety protocols in place to protect nurses and patients alike as a potential area for improvement through collaboration.
“We saw a lack of safe handling protocols,” Song said. “Although a special workstation for chemotherapy drug mixing was recently added, they lacked biohazard disposal for drugs, pregnant nurses were still mixing chemotherapy, and more. Providing education about safe handling is an area of opportunity to help make a difference.”
Sharing Resources to Effect Change
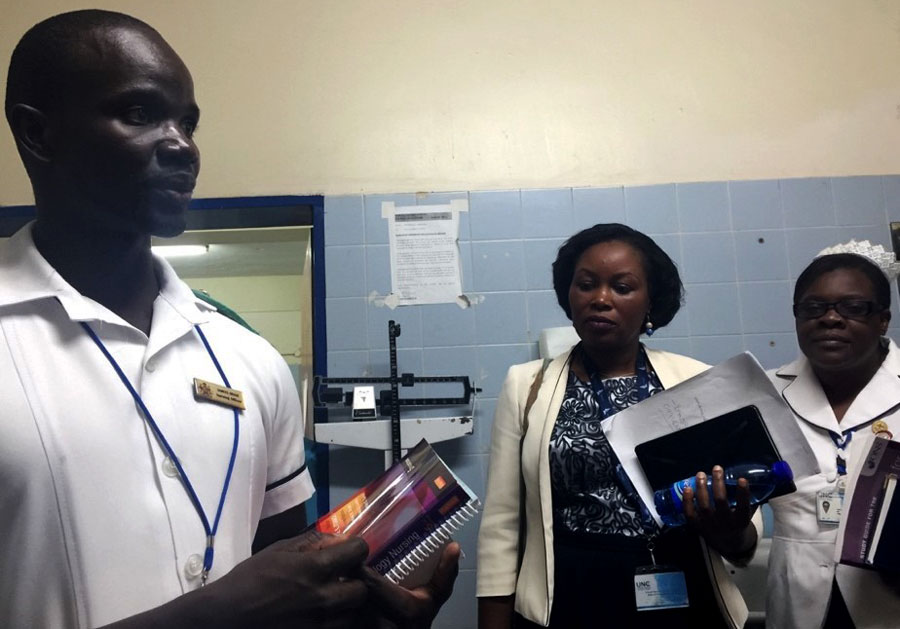
As part of ONS’s ongoing efforts to connect and support international oncology communities, the Society provided several oncology nursing books that Bryant, Song, and their colleagues delivered.
“Unfortunately, nurses in Lilongwe don’t have the most up-to-date guides, resources, and books for clinical practice, and that can really impact their ability to provide quality care to their patients,” Bryant explained. “Being able to provide a set of books to KCH and KCN meant a lot to the nursing educators, students, and oncology professionals. There’s currently only one oncology certified nurse in Lilongwe, and he was so pleased to have resources he could use for things like safe handling and symptom management.”
Other ONS resources helped Bryant, Song, and the team structure what they learned in Malawi to create an action plan to follow in the future.
“We’re pleased that ONS is a leader in global nursing care. The Society provided us with a need assessment framework that we were able to tailor to those working in Malawi,” Bryant says. “This was a major first step for us to get a better sense of the current state of care in the country. It helped us determine our next steps from a research and education perspective.”
Building a Plan for the Future
Through the needs assessment in Malawi, the team identified three areas for future growth and collaboration with their oncology nursing cohorts: develop short, modular basic oncology courses in conjunction with train-the-trainer programs; continue conversations between the team and members at KCH and KCN; and provide a nursing perspective to develop new research initiatives.
“Through the oncology courses, we’ll find champions at local hospitals,” Song says. “And with a train-the-trainer approach, we hope to help prepare more oncology nurses for practice through those local champions. I have already started mentoring some PhD-prepared nurses by reviewing their grant proposals, and we hope to get a pilot study running to lead research and education programs for the local nurses and their patients with cancer.”
Bryant said that they didn’t just stop once they learn about the gaps in care, but they are making plans for follow up and providing ongoing support to their colleagues in Malawi.
“One of our goals is not to just go in and say we’re going to do all these things for people and never come back,” Bryant said. “We’re planning e-learning programs for April 2019 to provide them with a better sense of oncology nursing care—similar to ONS’s Cancer Basics course. Then we’ll look to return in summer 2019 to do some hands-on learning for a minimum of two weeks. We’re also finding ways to have ongoing conversations with them through the year.”
For both Song and Bryant, their visit to Malawi has been an educational one, but the work is just getting started.
“It’s been an inspirational and humbling journey,” Song said. “We’ve seen a huge need, and it might seem impossible to close the gaps for these providers and their patients with cancer. But we have a plan and we are determined to get started one step at a time.”
Bryant encouraged her nurse colleagues to step into leadership roles and find ways to engage in international work.
“Look to the ONS global community and the other resources available to you,” Bryant says. “Understand the reason about why you’re there and the long-term goals. Nurses can help build the capacity of their international colleagues and really make a change for the betterment of care.”
