Cross-Discipline Cancer Care
Complex cancer treatments like bispecific antibodies (BsAbs) and chimeric antigen receptor (CAR) T-cell therapy are associated with equally complex side effects and complications. When patients experience signs and symptoms back home away from their dedicated cancer care team, how should they seek intervention? Should they go to the emergency room? The local urgent care facility? Call 9-1-1? And, if they do any of those things, will the healthcare providers in those settings know how to care for them?
Emergency Care, Urgent Care, and Cancer Care: Identifying the Difference
ONS member John Rodriguez, MA, MSN, RN, BMTCN®, OCN®, a staff nurse in the hematology/bone marrow transplant department at Huntsman Cancer Institute (HCI) in Salt Lake City, UT, cares for patients receiving BsAbs and participated in the ONS Bispecific Antibodies Focus Group.
HCI is a National Cancer Institute (NCI)-designated Comprehensive Cancer Center affiliated with the University of Utah. It serves a broad patient population, including individuals from as far away as Colorado, Montana, Idaho, Wyoming, and Nevada. Rodriguez said that some of his patients have traveled up to 800 miles to HCI because they require advanced or complex treatments that are not available at local hospitals or clinics. Once discharged, returning to HCI is no easy feat.
Rodriguez recognized two challenges for patients and healthcare professionals:
- Patients need to understand their treatments and what to watch for when they return home.
- Healthcare providers need to be able to collaborate across settings to manage potentially serious complications.
Rodriguez said that patients receiving BsAbs and other immunotherapies may have symptoms that are similar to those associated with graft-versus-host disease (GVHD), such as skin sensitivities and rashes, as well as ocular issues like blurred vision, light sensitivity, dry eyes, and inflammation. Gastrointestinal symptoms and signs of infection are also common side effects. However, side effects can be associated with many different conditions, so patients should start by contacting their oncology team. Non-oncology providers may not be equipped to manage complex conditions stemming from cancer or cancer treatments.
“The key is communication,” Rodriguez said. “Patients need to understand that if they have a fever, if they have nausea and can’t keep anything down, severe diarrhea, pain in the shoulder, things like that, they need to know when their symptoms require a call to their oncology care team.” Rodriguez said patients at HCI receive discharge instructions with information on common side effects and symptoms that indicate a need for urgent care. Instructions include a phone number to call to reach a provider who can advise whether they should go to the cancer clinic or emergency department.
HCI also serves Native American populations often located in rural or remote areas, requiring patients to travel significant distances to receive dedicated cancer care. Although HCI collaborates with Indian Health Service facilities or tribal health clinics, Rodriguez said that the community faces barriers such lack of health insurance coverage and other financial toxicities. Rodriguez’s team collaborates with a wide range of service providers, including transportation companies, to support patients in any community.
Rodriguez said that he tells patients to hand their patient information instructions to non-oncology healthcare professionals; that becomes particularly useful in emergency situations when patients cannot self-report information. Rodriguez said the instructions include thresholds and “watch-out” warnings for healthcare professionals to measure symptom severity. They also instruct cross-discipline professionals to contact the oncology team for more specialized instructions or to initiate a trip to HCI.
“People regularly come from several hours away,” Rodriguez said. “They might report to an emergency department in the middle of nowhere, and because of the distance and medical condition, they may be life-flighted to HCI. The goal is to determine if this is something requiring critically urgent care or something that can wait until their next visit. Our goal is to promote safety, informed decision-making, and proactive health management.”
In fact, Rodriguez said it is common for local emergency departments to call and say that a patient is on their way. “They will provide their vitals, and, while on the road, the transportation company continues to provide care and vitals so that as soon as they arrive, they can go right in and the treatment team is ready to provide care,” Rodriguez said.
“It isn’t possible for the emergency department to know how to do everything,” Rodriguez said. “There are so many treatments and so many variables.”

Interprofessional Partnerships Involve Planning, Protocols, and Patient Education
CAR T-cell therapy has transformed outcomes for many patients with hematologic malignancies, but because it is a specialized, complex treatment, its availability is largely limited to academic cancer centers. Toni Henderson-Clark, MS, MSBA, RN, is the director of patient care services at Karmanos Cancer Institute in Detroit, MI. The Karmanos Cancer Institute is an NCI-designated comprehensive cancer center. The cancer center and research institute serve the Detroit metropolitan area, representing the majority of Michigan’s population.
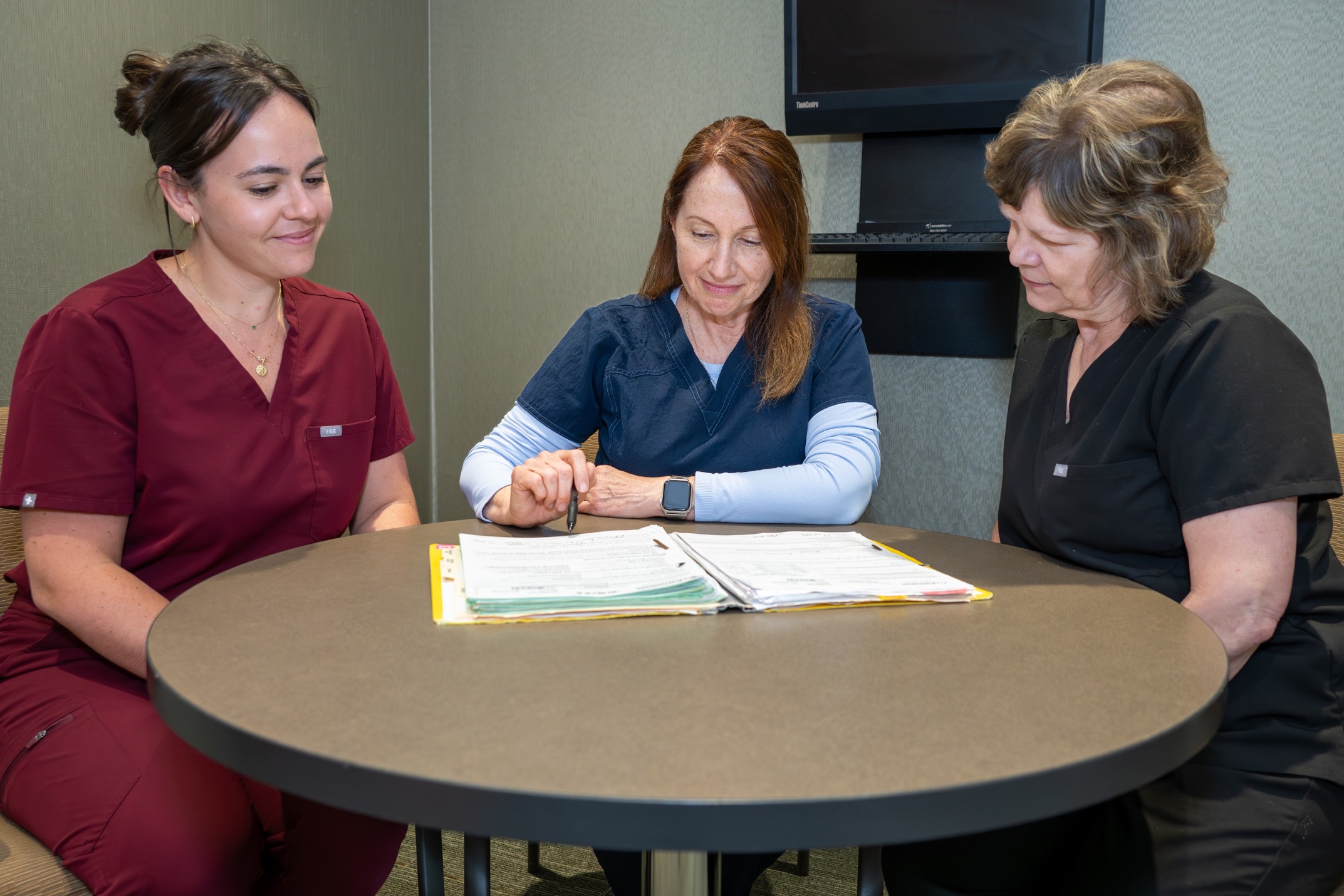
Henderson-Clark’s nursing background is in critical care and hematopoietic stem cell transplantation, and she is currently the primary contact for CAR T-cell therapy processes and the Foundation for the Accreditation of Cellular Therapy accreditation at Karmanos. She works with infusion, inpatient, and critical care departments and ambulatory clinics to provide multifaceted care to patients receiving CAR T-cell therapy.
“The oncology nurse’s role spans the continuum of care and includes clinician, coach, educator, and patient advocate,” she said.
Henderson-Clark said that her team most commonly supports other disciplines to manage cytokine release syndrome and neurotoxicities. Collaboration also includes ensuring non-oncology clinicians are well-versed in the goals of therapy, common side effects, and signs of an emergency.
“The oncology nurse serves as the content expert, process expert, mentor, and coach to the non-oncology practitioner,” she said.
Many safety protocols are implemented to ensure a patient’s journey is well-managed during the post–CAR T-cell therapy infusion phase of care. Henderson-Clark said that the center’s cellular therapy team, including physicians, advanced practice providers, nurse navigators or coordinators, infusion nurses, clinic and inpatient unit nurses, leaders, social workers, and finance, collaborated to develop the safety protocols.
Oncology nurses lead the collaborative team, whose work starts with identifying safety guidelines. A variety of oncology nurses actively participate in this process, including the oncology nurse coordinator, clinic nurse, clinical trials nurse, infusion nurse, and the cellular therapy infusion coordinator.
Patients must have an assigned, designated caregiver. Nurses teach patients and caregivers about the CAR T-cell therapy treatment plan. Patients learn how to contact the prescribing provider and to always carry the CAR T-cell therapy patient wallet card identifying the medication received, the date of the infusion, the prescribing provider’s contact information, and other crucial information.
“Managing the patient after hours is one of the most complex challenges we faced. Being an advanced practice nurse and nurse leader, I quickly identified this as a potential barrier and safety issue,” Henderson-Clark said. “We convened a core interprofessional team and designed an after-hours process to facilitate triaging and access to care at our center 24 hours a day during the critical monitoring timeframe. We developed an after-hours triage system that encompasses the attending physician, the hospitalist, an on-call nurse with specialty training with a second backup on-call nurse leader, nursing supervisor, and inpatient nursing personnel.”
Patients are taught to call their attending physician if they suspect adverse events. If telephone triage determines that the patient needs to be assessed in person, the attending physician alerts the on-call nurse who implements a “fan-out” process:
- The patient is provided access to the building, bypassing the emergency department.
- The hospitalist and a cellular therapy nurse conduct initial assessment, and the hospitalist collaborates with the attending physician.
- A mass communication is shared following triage assessment so that the team can appropriately direct its attention to the patient’s most current needs.
BsAb and CAR-T therapy also can be very costly, compounding patient access issues. Henderson-Clark said that having a system committed to raising awareness of and supporting diversity, implicit bias, disparity of care, and issues related to access helps to reduce some of those inequities.
“This infrastructure has assisted in fostering a heightened awareness among providers. I feel our team is better able to assess our patients’ needs and effectively problem-solve. This awareness has also forged a new sense of relatability,” she said.
To support interprofessional education and diversity, oncology nurses often attend healthcare community events where they can speak to non-oncology practitioners about new treatments. Non-oncology nurses are usually intrigued by the science and manufacturing involved, Henderson-Clark said.
“Often the word ‘cancer’ denotes end-of life to a non-oncology professional,” Henderson-Clark said. “In fact, our center’s goal is a world free of cancer. In the interim, as an oncology nurse, I strive to impress the importance of milestones, quality of life, self-advocacy, and self-determination.”
Henderson-Clark encouraged other oncology nurses to embrace collaboration and interprofessional care and to actively participate in ground-level work when designing a programmatic approach to oncology care. She suggested that teams consistently reevaluate and refine processes to adjust to the changing treatment landscape.
“Remember that your approach should be value-based and dynamic, just like the realm of oncology care,” she said.
