Use Conversational Assessments to Deliver Whole-Person Care
Whole-person care involves evaluating a patient’s physical, emotional, spiritual, and social health. A conversational assessment can help oncology nurses foster an open dialogue about the patient as a person, not just their physical or health needs.
Each wellness dimension of whole-person care is mutually dependent but not always equally balanced. For example, physical pain can affect emotions and vice versa. A conversational assessment can help oncology nurses collect information for standard assessment tools, such as the OLD CARTS pain assessment (an acronym for onset, location/radiation, duration, character, aggravating factors, relieving factors, timing, and severity). When you use it as a conversational assessment instead of a static checklist, OLD CARTS helps nurses identify anything that may have been missed during patient encounters.
Emergent and critical care assessments require a priority-focused assessment, however. Conversational assessments (https://doi.org/10.1111/nicc.12237) are most useful in less critical circumstances and generally not appropriate for emergency situations.
Apply It to Your Practice
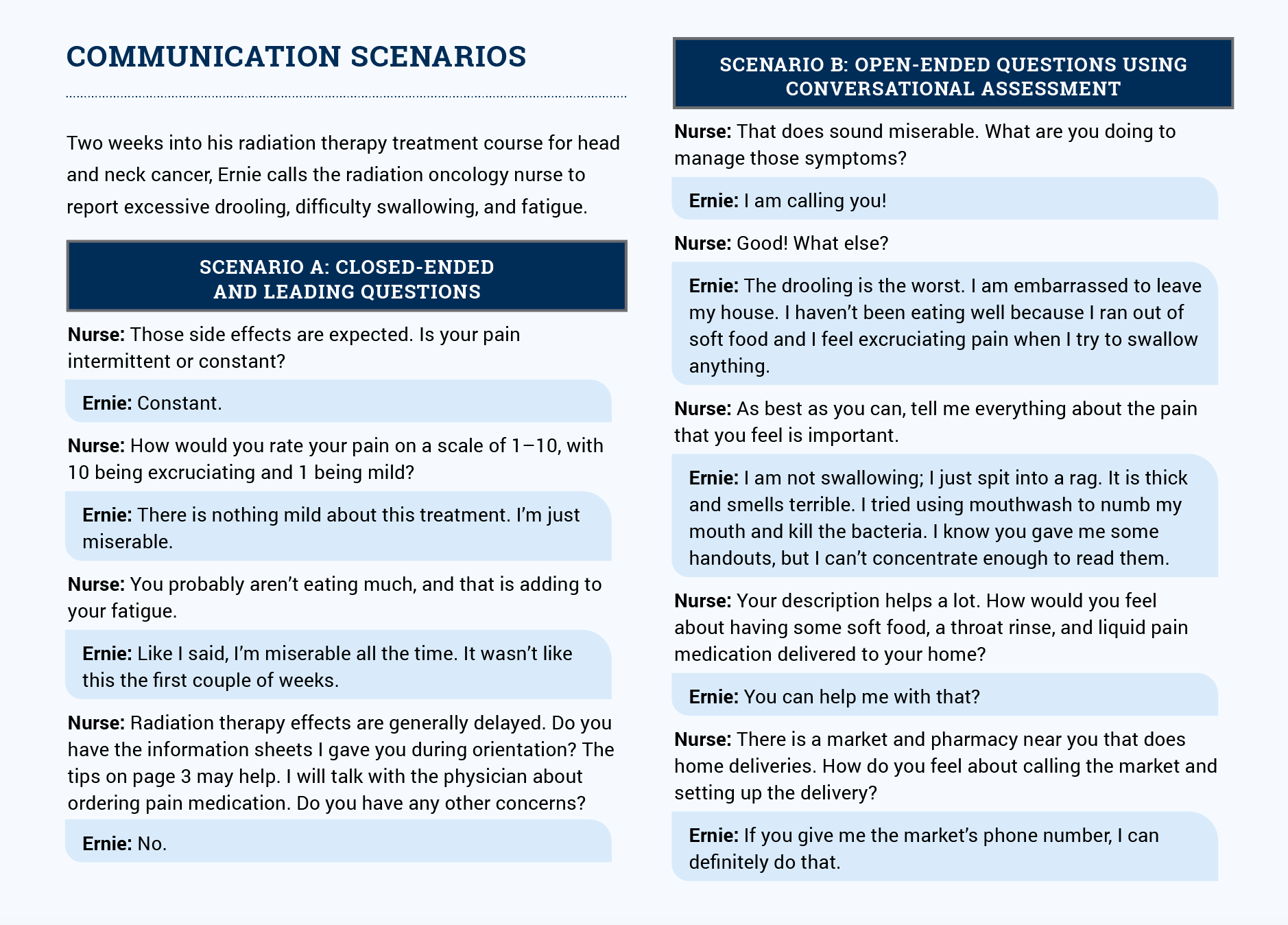
In scenario A in the sidebar, the nurse uses closed-ended and leading questions. Ernie does not open up much and the nurse misses exploring what miserable means to Ernie. In scenario B, the nurse prompts a conversation by using open-ended questions, validation, and listening for what Ernie doesn’t directly say. Based on his dialogue, the nurse concludes that Ernie is using alcohol-based mouthwash and realizes that handouts may not be an effective method of communication with him.