Nursing Considerations for Melanoma Survivorship Care
Breast, prostate, colorectal, and melanoma are the most common primary cancer sites (https://doi.org/10.6004/jnccn.2020.0037) among 58% of survivors. Advancements in immunotherapy and targeted therapies have significantly increased treatment options for a disease that once had very limited treatment options, markedly improving overall five-year survival rates (https://doi.org/10.1188/17.cjon.s4.7-10) for patients with melanoma. Yet survival rates vary (https://www.cancer.org/cancer/melanoma-skin-cancer/after-treatment/follow-up.html) depending on extent of disease (https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf) (local versus metastatic) and ethnic minority disparities. Although the overall (all stages combined) five-year survival rate for White patients with melanoma is 93%, the rate drops to 87% (https://doi.org/10.1016/j.jaad.2020.08.097) for Hispanics and to just 23% (https://www.cancer.org/cancer/melanoma-skin-cancer/detection-diagnosis-staging/survival-rates-for-melanoma-skin-cancer-by-stage.html) for those with distant melanoma.
Late and Long-Term Effects
Common late and long-term effects in melanoma survivors are largely dependent on the treatment modality, specific agents, and dosage. Most patients receive surgery, immunotherapy, targeted therapy, chemotherapy, or radiation. Patients who underwent complete lymph node dissection or excision or sentinel lymph node surgery may experience lymphedema (https://doi.org/10.6004/jnccn.2020.0037). ONS GuidelinesTM (http://ons.org/articles/ons-guidelinestm-cancer-treatment-related-lymphedema) provide evidence-based recommendations for lymphedema management. Chemotherapy and radiation side effects depend on agent, dose, or area of the body irradiated.
Immunotherapies, including checkpoint inhibitors such as ipilimumab, nivolumab, and pembrolizumab, are often first-line treatment (https://www.nccn.org/professionals/physician_gls/pdf/cutaneous_melanoma.pdf) in eligible patients. Checkpoint inhibitors are associated with immune-related adverse events (https://doi.org/10.1001/jamanetworkopen.2020.1611), including dermatitis, colitis, endocrinopathies (e.g., hypothyroidism), pneumonitis, and other inflammatory processes. Careful assessment and early intervention are critical for reducing long-term and permanent effects for melanoma survivors. Management of immune-related adverse events may include systemic corticosteroids, which are associated with additional long-term considerations for survivorship, such as evaluation for osteoporosis with a DEXA scan. Learn more (https://www.ons.org/webinars/corticosteroids-and-implications-long-term-immunosuppression-recorded-webinar) about the long-term effects of immunosuppression in patients with cancer.
Targeted therapy (https://www.cancer.org/cancer/melanoma-skin-cancer/after-treatment/follow-up.html) such as BRAF inhibitors (e.g., vemurafenib, dabrafenib, encorafenib) are another common treatment option (https://doi.org/10.6004/jnccn.2020.0037). The agents have specific acute side effects, but long-term organ toxicity (e.g., heart, lung, liver) must be monitored throughout survivorship. Common long-term concerns (https://doi.org/10.1007/s11764-019-00770-0) among melanoma survivors who receive immune checkpoint inhibitors and BRAF-MEK inhibitors are dry, itchy skin; arthralgias; fatigue; and psychological distress from fear of recurrence or death.
Screening and Prevention
Survivorship care plans should be tailored for specific patient factors, risks factors, comorbidities, and family history. Melanoma survivors require routine blood work with consideration for lipid panels and monitoring for secondary malignancies. Encourage healthy lifestyle behaviors, including regular exercise, smoking cessation, limited alcohol consumption, sun safety, and staying current with routine, age-appropriate cancer screening. Include a diet high in fruits, vegetables, and whole grains (https://www.cancer.org/cancer/melanoma-skin-cancer/after-treatment/follow-up.html) and low in fat, processed foods, and red meat (https://doi.org/10.6004/jnccn.2020.0037).
Sample Melanoma Survivorship Care Plan
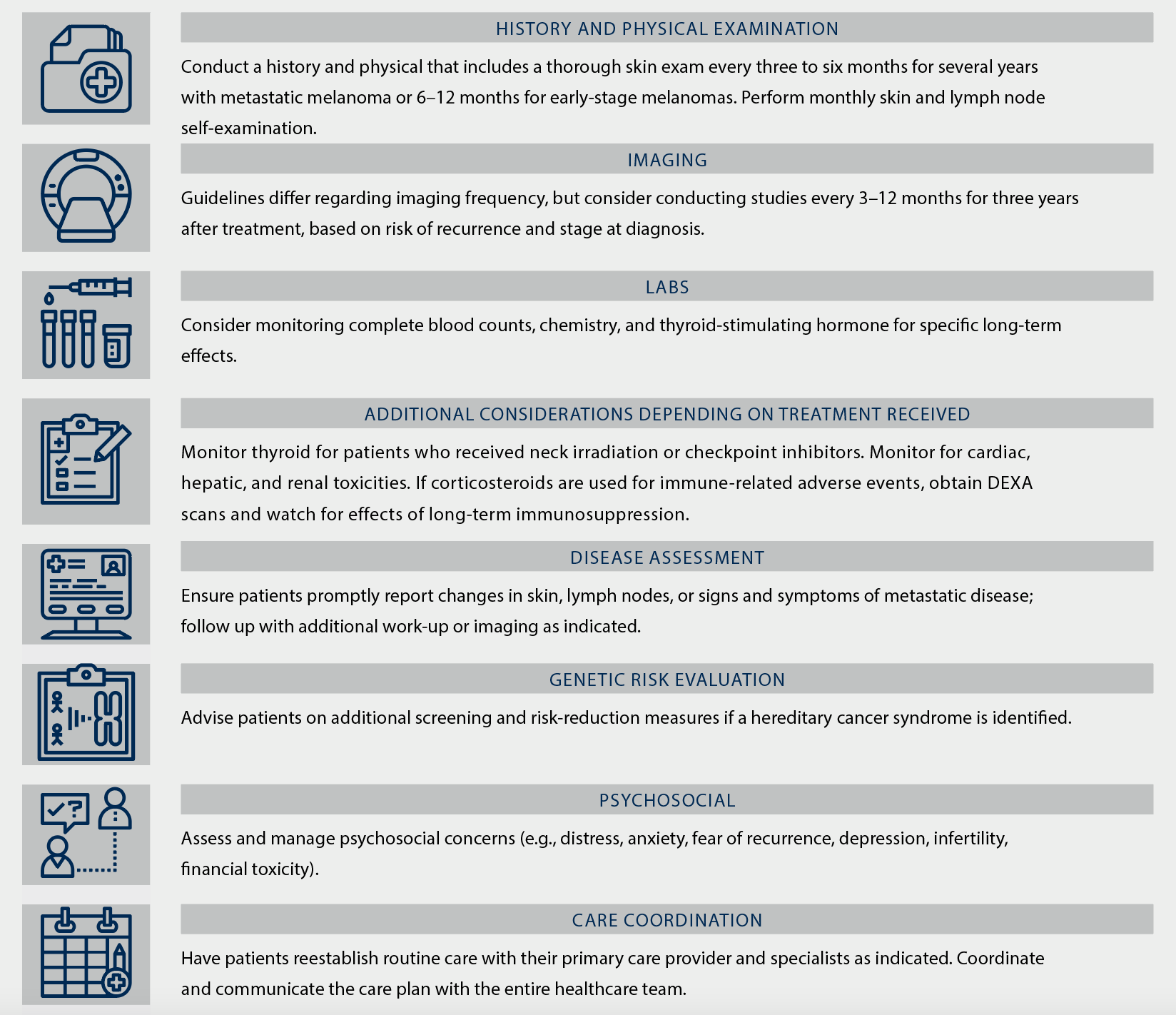
Note. Plans are largely determined based on disease stage. Based on information from ACS (https://www.cancer.org/cancer/melanoma-skin-cancer/after-treatment/follow-up.html), Freeman and Laks (https://doi.org/10.2217%2Fmmt-2019-0003), and Swetter et al (https://doi.org/10.1016/j.jaad.2018.08.055).
