Billing and Coding Breakdown Helps Nurses Recognize the Realities of Reimbursement
Understanding correct coding strategies is an important skill that affects billing and reimbursement for value-based cancer care. Meeting the requirements for complete and accurate documentation is critical to support healthcare claims. Both nurses and advanced practice providers (APPs) have responsibilities in this work.
Billing and coding requirements vary across states and individual practices because of federal laws, state regulations, payor contracts, and institutional policies. Oncology nurses should be aware of their state’s and institution’s regulations to avoid errors in billing and unnecessary loss of revenue or additional out-of-pocket expenses for patients.
Advanced Practice Providers
APP billing is either incident-to or independent. Incident-to billing is used (https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c15.pdf) when APPs perform the visit while the collaborating physician is in the office suite. The physician develops the treatment plan and supervises the APP. The physician is considered the billing provider and the APP is the rendering provider; in other words, the quality measures and care are credited to the physician, not the APP, and any bonus for the care goes to the physician. This situation is reimbursable (https://doi.org/10.1097/01.NPR.0000552680.76769.e5) at 100% of the allowable amount.
The APP may also use their own National Provider Identifier to bill Medicare independently, but the reimbursement is limited (https://doi.org/10.1097/01.NPR.0000552680.76769.e5) to 85% of the full allowable physician payment. Private payor contracts generally vary in rates of APP reimbursement.
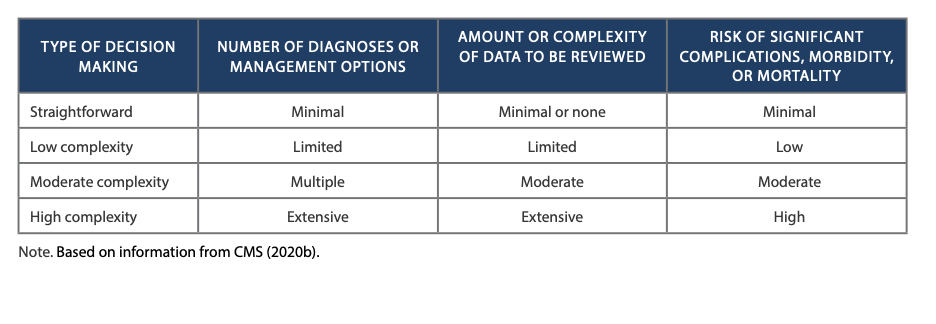
Coding for an established patient visit requires three key components (https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Medicare-Information-for-APRNs-AAs-PAs-Booklet-ICN-901623.pdf), or evaluation and management (E/M) services: history, examination, and medical decision making. APPs must fully document two of the three key components to bill for an established patient visit. Alternatively, APPs can bill (https://www.cms.gov/Outreach-and-Education/Outreach/Partnerships/downloads/providerbillingforcaregivereducation.pdf) for time spent and documented in counseling or care coordination for a particular level of E/M service. For example, 99213 = 15 minutes, 99214 = 25 minutes, and 99215 = 40 minutes. The documentation should read “greater than 50% of the face-to-face time was spent discussing the above (i.e., your documentation). 20/25 minutes was spent.” This would be billed as 99214.
RNs’ Role in Reimbursement
Oncology RNs educate patients frequently, but that work is not typically supported by formal reimbursement. Tara Sweeney, BSN, RN, OCN®, CHPN, a nurse navigator from Main Line Health in Paoli, PA, said that she is able to code for chemotherapy and treatment education visits using the 99211 E/M code: “an office visit for the evaluation and management of an established patient that may not require the presence of a physician.” However, RN billing is always incident (https://www.aafp.org/journals/fpm/blogs/inpractice/entry/coding_99211.html) to either a physician or a nurse practitioner and cannot be billed (https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c15.pdf) on the same day as another provider visit; the higher provider prevails in billing.
Other situations that are billable by an RN or APP, based on medical decision making or time spent in care coordination and counseling, include:
- Survivorship care plan review
- Chronic care management (e.g., phone calls, referrals to visiting nurse associations or other providers, review of radiology tests with radiologist, review of laboratory results)
- Oral therapy education
- Assessment of adherence to oral therapies
- Toxicity monitoring
- Symptom management
“We are constantly educating our patients among many other tasks, and it is more prevalent a need for us to capture value in this current pandemic climate,” Sweeney said. She added that the visits that are coded and billed tend to have more supporting documentation, which improves the medical record and communication between clinicians.
Learning the fundamentals of billing, coding, and reimbursement gives RNs and APPs greater opportunities to support the contributions and value of their work in the delivery of comprehensive cancer care.
