The state of Kentucky has seen some of the most success in reducing its uninsured rate thanks to the Affordable Care Act’s Medicaid expansion that took effect on January 1, 2014. The results of a new study, published in the Journal of the American College of Surgeons, showed that as the number of insured individuals rose, so too did important cancer screening rates.
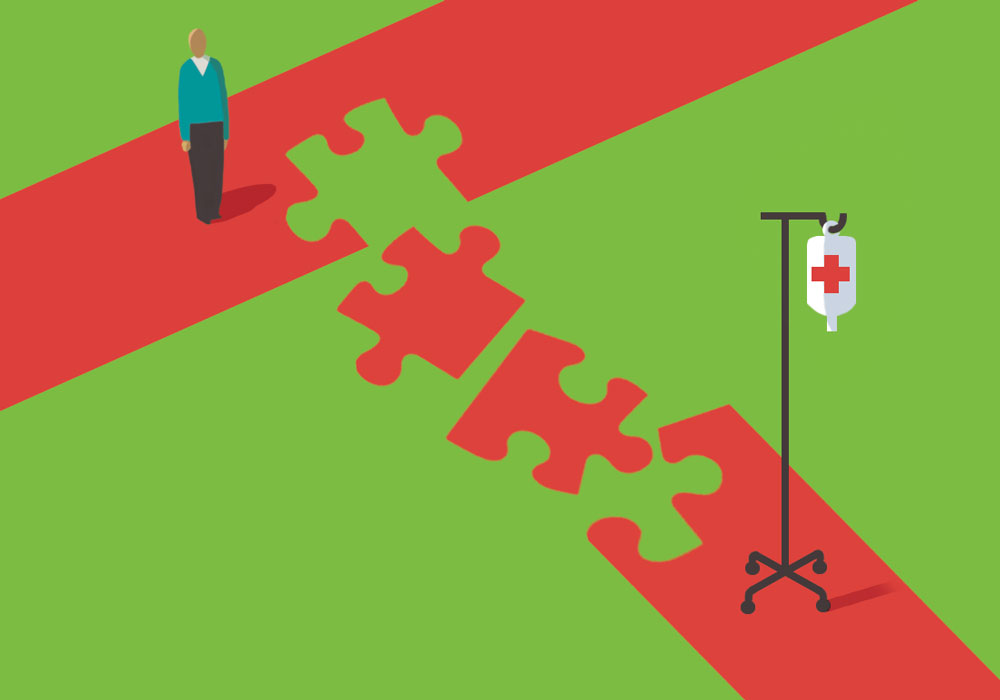
Historically, Kentucky had a low screening rate for colorectal cancer (CRC), which has led to high CRC incidence and mortality rates in the state. When Medicaid expansion was enacted, an additional 635,807 low-income patients gained access.
Researchers looked at data from the Kentucky Hospital Discharge Database and Kentucky Cancer Registry and found that after Medicaid expansion, an additional 113,176 patients with any type of insurance coverage underwent CRC screening. More than half (67,230 patients) were covered under Medicaid—an increase of 230% in that group alone.
The researchers also identified that CRC diagnoses increased by 132.4% but couldn’t explain the finding; however, they noted that long-term data observation should see a reduced rate in the future.